Hospital-Wide Healthcare-associated Bloodstream Infections Surveillance results: 2016-2017

From April 1st, 2016, to March 31st, 2017, 89 healthcare facilities took part in the hospital-wide surveillance of bloodstream infections (BSIs), for a combined total of 4,830,348 patient days (Table 1). Participating facilities reported 3,167 BSIs in 2,982 patients. The total incidence rate was 5.43 cases per 10,000 patient days. The incidence rate in 2016–2017 is stable compared with the average rate for 2012–2016. Two non-teaching facilities joined the program in 2016–2017. Data were extracted on May 5th, 2017.
Update: October 5, 2017
Version française
Table 1 – Participation of Healthcare Facilities in the Hospital-Wide Surveillance of BSIs, Québec, 2012–2013 to 2016–2017
2012-2013 | 2013-2014 | 2014-2015 | 2015-2016 | 2016-2017 | |
|---|---|---|---|---|---|
| Participating facilities (N) | 64 | 73 | 89 | 87 | 89 |
| Admissions (N) | 482,354 | 520,772 | 633,252 | 649,458 | 677,083 |
| Patient days (N) | 3,791,482 | 3,998,173 | 4,740,371 | 4,771,179 | 4,830,348 |
| BSIs (cat. 1a, 1b and 1c, N) | 2,537 | 2,457 | 3,008 | 3,126 | 3,167 |
| Infected patients (N) | 2,428 | 2,295 | 2,806 | 2,899 | 2,982 |
Incidence rates
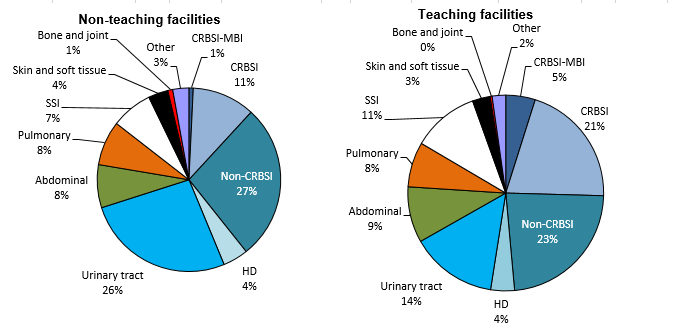
In 2016–2017, the total incidence rate is 5.43 BSIs per 10,000 patient days. The incidence rates remain much higher in intensive care units (ICUs) than in other units (Table 2). They are also higher in teaching facilities than in non-teaching facilities (Figure 1 and Table 2). Catheter-related bloodstream infections (CRBSIs) are the most common BSIs in teaching ICUs; in non-teaching ICUs, it is rather non-catheter-related primary bloodstream infection (non-CRBSI) (Figure 2). In other units, the incidence rates also vary depending on the type of healthcare facility: non-CRBSI are the most common BSIs in teaching facilities, while BSIs secondary to urinary tract infections are the most common in non-teaching facilities (Figure 3). In teaching facilities, in non-intensive care units, the CRBSI incidence rate (1.11 case / 10,000 patient days) increases to 1.54 case / 10,000 patient days when CRBSI associated with a mucosal barrier injury (MBI) are also considered (Figure 3 and Table 2).
Figure 1 – BSI Incidence Rate for Each Type of Infection, by Type of Healthcare Facility, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
Figure 2 – BSI Incidence Rate in ICUs, For Each Type of Infection, by Type of Healthcare Facility and Type of ICU, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
Figure 3 – BSI Incidence Rate in Non-ICU Units, for Each Type of Infection, by Type of Healthcare Facility, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
Table 2 – BSI Incidence Rate for Each Type of Infection, by Type of Healthcare Facility, Type of Unit and Type of ICU, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
| Primary BSIs | Secondary BSIs | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
CRBSI-MBI | CRBSI | Non-CRBSI | HD | Urinary tract | Abdominal | Pulmonary | SSI | Other** | ||
| Total hospitalized | 0.22 | 0.96 | 1.16 | 0.04 | 1.08 | 0.54 | 0.49 | 0.59 | 0.35 | 5.43 |
| Teaching | 0.41 | 1.53 | 1.49 | 0.06 | 1.20 | 0.79 | 0.65 | 0.92 | 0.43 | 7.47 |
| Non-teaching | 0.03 | 0.40 | 0.84 | 0.01 | 0.97 | 0.30 | 0.32 | 0.27 | 0.27 | 3.42 |
| ICUs | 0.19 | 4.66 | 2.43 | 0.06 | 1.24 | 1.34 | 2.36 | 1.18 | 0.59 | 14.05 |
| Adult teaching | 0.15 | 3.88 | 2.49 | 0.15 | 1.76 | 1.17 | 3.30 | 2.20 | 0.88 | 15.97 |
| Adult non-teaching | 0.11 | 2.58 | 3.37 | - | 1.68 | 1.12 | 2.58 | 0.67 | 0.45 | 12.56 |
| Pediatric | 1.50 | 14.21 | 2.24 | - | - | 0.75 | - | 0.75 | 0.75 | 20.20 |
| Neonatal | 0.12 | 6.65 | 1.33 | - | 0.12 | 1.94 | 0.97 | 0.12 | 0.24 | 11.49 |
| Non ICU units | 0.22 | 0.70 | 1.07 | 0.03 | 1.07 | 0.48 | 0.35 | 0.55 | 0.33 | 4.81 |
| Teaching | 0.43 | 1.11 | 1.43 | 0.06 | 1.21 | 0.72 | 0.48 | 0.87 | 0.40 | 6.70 |
| Non-teaching | 0.03 | 0.32 | 0.75 | 0.01 | 0.95 | 0.26 | 0.24 | 0.26 | 0.26 | 3.07 |
* When the incidence rate is 0, the confidence interval [CI] is not calculated.
** The “Other” column also includes HD-related BSIs and secondary BSIs arising from a skin, soft tissue, bone or joint infection.
Incidence rate time trends
The BSI incidence rate in 2016–2017 remains stable compared with the 2012–2016 pooled rate (p > 0.05, Table 3). This is observed in both teaching and non-teaching facilities. This stability is also observed for every BSI type except for non-CRBSIs and BSIs secondary to an abdominal infection (p < 0.05, Figure 4). The apparent variation in rates of BSIs secondary to a urinary infection is not statistically significant.
Figure 4 – Evolution of BSI Incidence Rates, by Type of Infection, in Facilities that Previously participated in Surveillance (N = 89), Québec, 2012–2016 and 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
Table 3 – Evolution of BSI Incidence Rates, by Type of Healthcare Facility, in Facilities that Previously participated in Surveillance (N = 89), Québec, 2012–2016 and 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
| Facility | Number of facilities | Incidence rate | |
|---|---|---|---|
2012-2013 | 2016-2017 | ||
| Teaching | 26 | 7.20 [7.02 ; 7.38] | 7.47 [7.14 ; 7.83] |
| Non-teaching | 63 | 3.49 [3.36 ; 3.61] | 3.43 [3.20 ; 3.67] |
| Total | 89 | 5.35 [5.24 ; 5.46] | 5.43 [5.23 ; 5.64] |
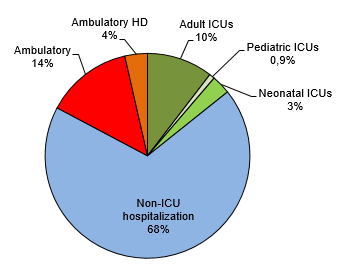
Description of cases
Patients who developed a BSI are aged between 0 and 101 years, with a median age of 69 years. Forty-one percent of BSIs (41%) occurred in women. Although the incidence rates are higher in ICUs, most BSIs occurred in non-ICU units (68%, Table 4 and Figure 5). Non-CRBSIs are the most commonly encountered BSIs in both teaching and non-teaching facilities (Table 4 and Figure 6).
Figure 5 – Breakdown of Cases Based on Type of Unit and Type of ICU, Québec, 2016–2017 (%)
Figure 6 – Breakdown of Cases Based on Type of BSI, for Teaching and Non-Teaching Healthcare Facilities, Québec, 2016–2017 (%)
Table 4 – Number of Cases for Each Type of BSI, by Type of Healthcare Facility, Type of Unit and Type of ICU, Québec, 2016–2017 (N)
| Primary BSIs | Secondary BSIs | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
CRBSI-MBI | CRBSI | Non-CRBSI | HD | Urinary tract | Abdominal | Pulmonary | SSI | Other* | ||
| Total | 111 | 551 | 778 | 130 | 580 | 275 | 240 | 310 | 192 | 3,167 |
| Teaching | 103 | 434 | 488 | 83 | 302 | 195 | 157 | 233 | 116 | 2,111 |
| Non-teaching | 8 | 117 | 290 | 47 | 278 | 80 | 83 | 77 | 76 | 1,056 |
| Total hospitalized | 106 | 465 | 561 | 17 | 523 | 260 | 235 | 286 | 168 | 2,621 |
| Teaching | 99 | 367 | 356 | 15 | 286 | 188 | 156 | 219 | 102 | 1,788 |
| Non-teaching | 7 | 98 | 205 | 2 | 237 | 72 | 79 | 67 | 66 | 833 |
| ICU | 6 | 150 | 78 | 2 | 40 | 42 | 78 | 38 | 19 | 452 |
| Teaching | 2 | 53 | 34 | 2 | 24 | 16 | 45 | 30 | 12 | 218 |
| Non-teaching | 1 | 23 | 30 | 0 | 15 | 10 | 23 | 6 | 4 | 112 |
| pédiatriques | 2 | 19 | 3 | 0 | 0 | 1 | 0 | 1 | 1 | 27 |
| néonatales | 1 | 55 | 11 | 0 | 1 | 16 | 8 | 1 | 2 | 95 |
| Non-ICU hospitalization | 100 | 315 | 483 | 15 | 483 | 217 | 159 | 248 | 149 | 2,169 |
| Teaching | 94 | 240 | 308 | 13 | 261 | 155 | 103 | 187 | 87 | 1,448 |
| Non-teaching | 6 | 75 | 175 | 2 | 222 | 62 | 56 | 61 | 62 | 721 |
| Ambulatory | 5 | 86 | 217 | 113 | 57 | 15 | 5 | 24 | 24 | 546 |
| Teaching | 4 | 67 | 132 | 68 | 16 | 7 | 1 | 14 | 14 | 323 |
| Non-teaching | 1 | 19 | 85 | 45 | 41 | 8 | 4 | 10 | 10 | 223 |
* The “Other” column also includes BSIs secondary to skin, soft tissue, bone or joint infection.
Three hundred and thirty four (334) procedures that occurred in the seven days preceeding the BSI are reported for the 778 non-CRBSIs (Table 5). Urologic procedures are the most frequently reported procedures, representing 42% of all reported procedures.
Table 5 – Distribution of Invasive Procedures Reported for Non-CRBSIs, by Type, Québec, 2016-2017 (N, %)
Type of invasive procedure | Procedures | |
|---|---|---|
N | % | |
| Urologic | 141 | 42.2 |
| Prostate biopsy | 47 | 14.1 |
| Ureteral double J stent placement | 47 | 14.1 |
| Cystoscopy / retrograde ureteroscopy | 32 | 9.6 |
| Percutaneous nephrostomy | 15 | 4.5 |
| Abdominal | 39 | 11.7 |
| Colonoscopy | 10 | 3 |
| Upper gastrointestinal endoscopy | 8 | 2.4 |
| Paracentesis – Ascitic tap | 10 | 3 |
| Other abdominal | 11 | 3.3 |
| Cardiovascular | 16 | 4.8 |
| Angiography with / without angioplasty or stent | 9 | 2.7 |
| Other cardiovascular | 7 | 2.1 |
| Hepatobiliary | 62 | 18.6 |
| ERCP with / without biliary stent | 59 | 17.7 |
| Other hepatobiliary | 3 | 0.9 |
| Musculoskeletal | 0 | 0 |
| Arthrocentesis (joint tap) | 0 | 0 |
| Cutaneous | 0 | 0 |
| Gynecological | 0 | 0 |
| Neurologic | 0 | 0 |
| Respiratory | 9 | 2.7 |
| Other | 67 | 20.1 |
| Total | 334 | 100 |
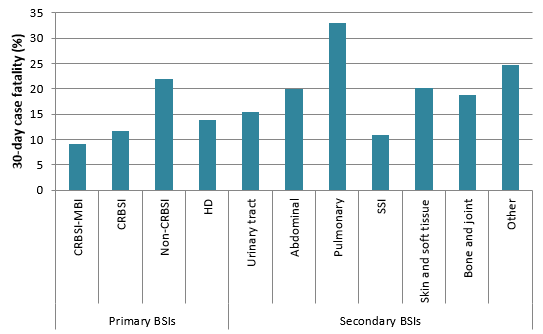
Overall, 18% of BSI cases resulted in death within 30 days of bacteremia onset (Table 6). Case fatality is highest in patients with a BSI secondary to a pulmonary infection (Table 6 and Figure 7).
Figure 7 – 30-Day Case Fatality for Each Type of Infection, Québec, 2016–2017 (%)
Table 6 – 10-Day and 30-Day Case Fatality for Each Type of Infection, 2016–2017 (N, %)
| BSIS | 10-day case fatality | 30-day case fatality | ||
|---|---|---|---|---|---|
(n) | n | % | n | % | |
| Primary BSIs | |||||
| CRBSI-MBI | 111 | 6 | 5 | 10 | 9 |
| CRBSI | 551 | 32 | 6 | 64 | 12 |
| Non-CRBSI | 778 | 127 | 16 | 171 | 22 |
| HD | 130 | 9 | 7 | 18 | 14 |
| Secondary BSIs | |||||
| Urinary tract | 580 | 48 | 8 | 89 | 15 |
| Abdominal | 275 | 38 | 14 | 55 | 20 |
| Pulmonary | 240 | 61 | 25 | 79 | 33 |
| SSI | 310 | 17 | 5 | 34 | 11 |
| Skin and soft tissue | 99 | 12 | 12 | 20 | 20 |
| Bone and joint | 16 | 1 | 6 | 3 | 19 |
| Other | 77 | 8 | 10 | 19 | 25 |
| Total | 3,167 | 359 | 11 | 562 | 18 |
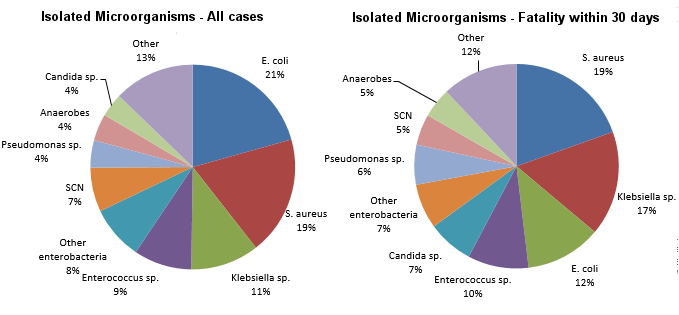
Microbiology
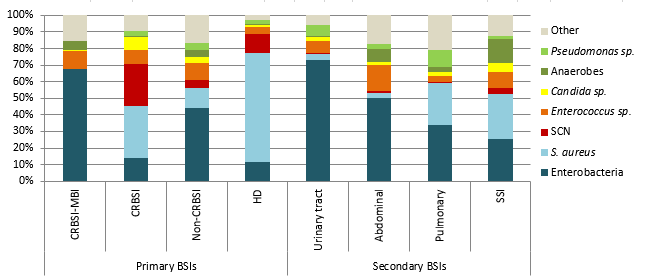
The three most frequently isolated microorganisms in reported cases and in cases resulting in death within 30 days are Escherichia coli, Staphylococcus aureus and Klebsiella sp. (Figure 8 and Table 7). Staphylococcus aureus is the most frequently isolated microorganisms in patients with CRBSIs, hemodialysis-related BSIs and in BSIs secondary to a pulmonary infection or a SSI (Figure 9 and Table 7). In patients with a non-CRBSI, CRBSI-MBI or a BSI secondary to a urinary tract or abdominal infection, Escherichia coli is the most common microorganism. A polymicrobial infection occurred in 11% of cases; this proportion reaches 21% in BSIs secondary to an abdominal infection and 14% in BSIs secondary to a SSI.
Figure 8 – Breakdown of Categories of Isolated Microorganisms in All Cases (N = 3,579) and Cases of Fatality Within 30 Days (N = 635), Québec, 2016–2017 (%)
Figure 9 – Breakdown of Categories of Isolated Microorganisms, for Each Type of BSI, Québec, 2016–2017 (%)
Table 7 – Breakdown of Microorganisms associated with BSIs, for each Type of BSI, for all BSIs and for those associated with a Fatality Within 30 Days, Québec, 2016–2017 (N, %)
| Microorganism | Primary BSIs | Secondary BSIs | Overall* | 30-day case fatality | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
CRBSI-MBI | CRBSI | Non-CRBSI | HD | Urinary tract | Abdominal | Pulmonary | SSI | n | % | ||
| Enterobacteria | 82 | 86 | 395 | 15 | 458 | 176 | 88 | 92 | 1431 | 226 | 15.8 |
| E. coli | 44 | 19 | 205 | 3 | 282 | 88 | 26 | 55 | 739 | 76 | 10.3 |
| Klebsiella sp. | 24 | 36 | 115 | 2 | 97 | 50 | 34 | 21 | 387 | 105 | 27.1 |
| Other enterobacteria | 14 | 31 | 75 | 10 | 79 | 38 | 28 | 16 | 305 | 45 | 14.8 |
| S. aureus | 0 | 195 | 111 | 87 | 23 | 10 | 66 | 98 | 672 | 124 | 18.5 |
| CNS | 0 | 158 | 41 | 15 | 5 | 5 | 1 | 13 | 250 | 31 | 12.4 |
| Enterococcus sp. | 13 | 55 | 95 | 6 | 45 | 55 | 10 | 35 | 328 | 61 | 18.6 |
| Candida sp. | 1 | 48 | 31 | 1 | 16 | 6 | 7 | 19 | 133 | 47 | 35.3 |
| Anaerobic | 6 | 2 | 35 | 1 | 2 | 28 | 7 | 52 | 152 | 30 | 19.7 |
| Pseudomonas sp. | 0 | 22 | 42 | 3 | 42 | 9 | 26 | 7 | 155 | 40 | 25.8 |
| Other | 19 | 57 | 148 | 4 | 37 | 61 | 55 | 44 | 458 | 76 | 16.6 |
| Total | 121 | 623 | 898 | 132 | 628 | 350 | 260 | 360 | 3579 | 635 | 17.7 |
* This column includes the sum of the other columns as well as secondary BSIs arising from a skin, soft tissue, bone or joint infection, or another source.
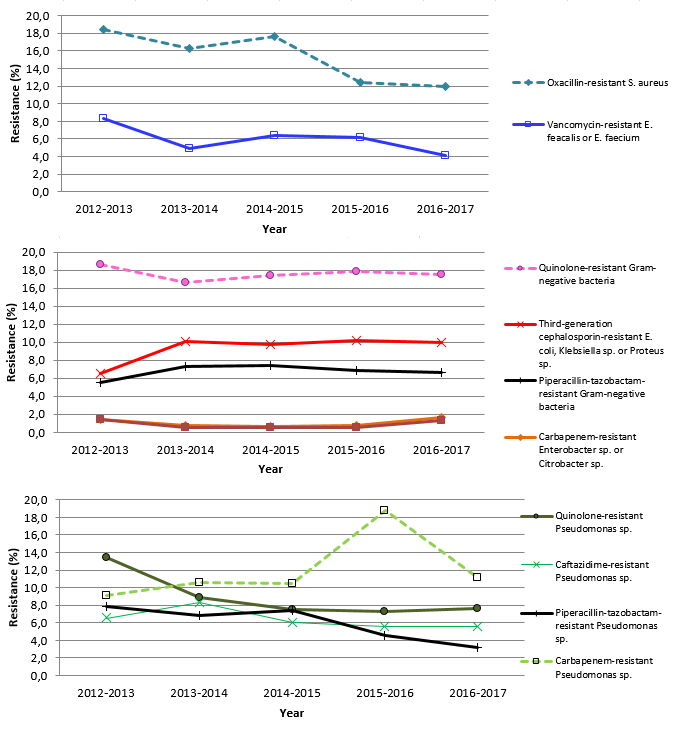
Methicillin-resistant S. aureus (MRSA) account for 12% (80 / 671) of S. aureus BSIs in all geographic areas (Table 8 and Figure 10); this represents a significant decrease compared to the 2012-2016 proportion (16%, p < 0.05). BSIs associated with carbapenem-resistant enterobacteriaceae continue to be relatively rare in Québec (13 / 997 or 1% of tested strains) and the apparent increase in resistance in 2015-2016 and 2016-2017 is not statistically significant. Please note that results presented in the second graph of Figure 10 exclude Pseudomonas sp.
Table 8 – Proportion of Strains Tested and Proportion of Resistance to Antibiotics for Selected Isolated Microorganisms, Québec, 2016–2017 (N, %)
| Microorganism | Antibiotic | Isolated | Tested | Resistant | ||
|---|---|---|---|---|---|---|
N | N | % | N | % | ||
| Staphylococcus aureus | Oxacillin | 672 | 671 | 99.9 | 80 | 11.9 |
| Enterococcus faecium | Vancomycin | 109 | 108 | 99.1 | 11 | 10.2 |
| Enterococcus faecalis | Vancomycin | 180 | 180 | 100 | 1 | 0.6 |
| Klebsiella sp. | CSE 4 | 387 | 294 | 76 | 22 | 7.5 |
| Imipenem ou meropenem | 387 | 257 | 66.4 | 3 | 1.2 | |
| Multiresistant 1 | 387 | 327 | 84.5 | 5 | 1.5 | |
| Escherichia coli | CSE 4 | 739 | 590 | 79.8 | 67 | 11.4 |
| Fluoroquinolones 3 | 739 | 669 | 90.5 | 188 | 28.1 | |
| Imipenem ou meropenem | 739 | 520 | 70.4 | 2 | 0.4 | |
| Multiresistant 1 | 739 | 657 | 88.9 | 26 | 4 | |
| Enterobacter sp. | CSE 4 | 122 | 93 | 76.2 | 26 | 28 |
| Imipenem ou meropenem | 122 | 97 | 79.5 | 2 | 2.1 | |
| Multiresistant 1 | 122 | 93 | 76.2 | 3 | 3.2 | |
| Pseudomonas sp. | Amikacin, gentamicin or tobramycin | 155 | 125 | 80.6 | 4 | 3.2 |
| CSE 2 | 155 | 144 | 92.9 | 8 | 5.6 | |
| Fluoroquinolones 2 | 155 | 145 | 93.5 | 11 | 7.6 | |
| Imipenem ou meropenem | 155 | 134 | 86.5 | 15 | 11.2 | |
| Piperacillin/tazobactam | 155 | 128 | 82.6 | 4 | 3.1 | |
| Multiresistant 2 | 155 | 146 | 94.2 | 9 | 6.2 | |
| Acinetobacter sp. | Imipenem ou meropenem | 14 | 12 | 85.7 | 1 | 8.3 |
| Multiresistant 3 | 14 | 6 | 42.9 | 0 | 0 | |
CSE 2: cefepime or ceftazidime;
CSE 4: cefepime, cefotaxime, ceftazidime or ceftriaxone;
Fluoroquinolones 2: ciprofloxacin or levofloxacin;
Fluoroquinolones 3: ciprofloxacin, levofloxacin or moxifloxacin;
Multiresistant 1: intermediate or resistant to an agent in three of the following five categories: cephalosporins 4, fluoroquinolones 3, aminoglycosides, carbapenems, piperacillin or piperacillin/tazobactam.
Multiresistant 2: intermediate or resistant to an agent in three of the following five categories: cephalosporins 2, fluoroquinolones 2, aminoglycosides, carbapenems, piperacillin or piperacillin/tazobactam.
Multiresistant 3: intermediate or resistant to an agent in three of the following six categories: cephalosporins 2, fluoroquinolones 2, aminoglycosides, carbapenems, piperacillin or piperacillin/tazobactam, ampicillin/sulbactam.
Figure 10 – Antibiotic Resistance in Gram-Positive Bacteria, Gram-Negative Bacteria and Pseudomonas sp., Québec, 2012–2013 to 2016–2017 (%)
Results per Healthcare Facility
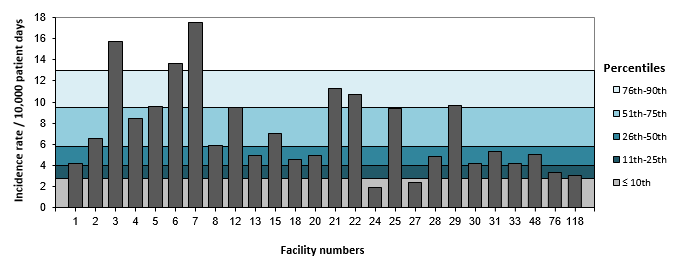
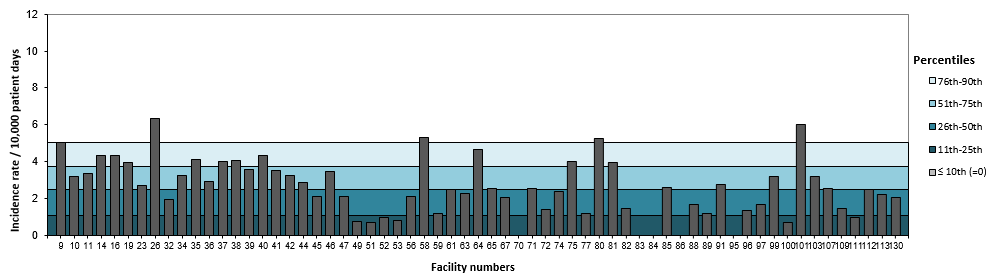
Three teaching and four non-teaching facilities have an incidence rate above the 90th percentiles of 2012-2016 incidence rates (Figures 11 and 12). Tables 9 and 10 present 2016-2017 rates of CRBSI and of BSIs secondary to urinary tract infections and SSIs, per healthcare facility.
Figure 11 – BSI Incidence Rate per Facility (2016–2017) and Percentile Ranking (2012–2013 to 2015–2016) for Teaching Healthcare Facilities, Québec, 2016–2017
Figure 12 – BSI Incidence Rate per Facility (2016–2017) and Percentile Ranking (2012–2013 to 2015–2016) for Non-Teaching Healthcare Facilities, Québec, 2016–2017
Table 9 – Incidence Rates of CRBSI and of BSIs Secondary to Urinary Tract and Pulmonary Infections per Facility and Percentile Ranking, for Teaching Healthcare Facilities, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
| Facility | CRBSI | Urinairy tract | SSI | ||||
|---|---|---|---|---|---|---|---|
Cases (n) | Incidence rates | Cases (n) | Incidence rates | Cases (n) | Incidence rates | ||
| 1 | HÔPITAL CHARLES LEMOYNE | 5 | 0.39 [0.16 - 0.94] | 5 | 0.39 [0.16 - 0.94] | 7 | 0.55 [0.26 - 1.15] |
| 2 | HÔPITAL DE L'ENFANT-JÉSUS | 19 | 1.46 [0.93 - 2.29] | 10 | 0.77 [0.41 - 1.43] | 7 | 0.54 [0.26 - 1.13] |
| 3 | GLEN - ROYAL VICTORIA | 35 | 3.24 [2.33 - 4.51] | 20 | 1.85 [1.19 - 2.87] | 22 | 2.04 [1.34 - 3.09] |
| 4 | HÔPITAL NOTRE-DAME DU CHUM | 23 | 2.21 [1.47 - 3.32] | 14 | 1.34 [0.80 2.27] | 11 | 1.06 [0.58 - 1.91] |
| 5 | HÔPITAL GÉNÉRAL JUIF | 31 | 1.84 [1.29 - 2.61] | 32 | 1.9 [1.34 - 2.68] | 7 | 0.42 [0.20 0.87] |
| 6 | GLEN - ENFANTS | 44 | 10.34 [7.70 13.9] | 1 | 0.24 [0.03 - 1.67] | 0 | 0 |
| 7 | PAVILLON L'HÔTEL-DIEU DE QUÉBEC | 14 | 1.65 [0.98 - 2.79] | 29 | 3.42 [2.38 - 4.93] | 22 | 2.6 [1.71 - 3.94] |
| 8 | PAVILLON MAISONNEUVE/PAVILLON MARCEL-LAMOUREUX | 28 | 1.5 [1.04 - 2.17] | 15 | 0.8 [0.48 - 1.33] | 13 | 0.7 [0.40 1.20] |
| 12 | CENTRE HOSPITALIER UNIVERSITAIRE SAINTE-JUSTINE | 45 | 5.15 [3.84 - 6.90] | 3 | 0.34 [0.11 - 1.06] | 2 | 0.23 [0.06 - 0.91] |
| 13 | INSTITUT DE CARDIOLOGIE DE MONTRÉAL | 3 | 0.67 [0.22 - 2.09] | 4 | 0.9 [0.34 - 2.40] | 8 | 1.8 [0.90 3.60] |
| 15 | HÔPITAL FLEURIMONT | 17 | 1.61 [1.00 2.59] | 8 | 0.76 [0.38 - 1.51] | 7 | 0.66 [0.32 - 1.39] |
| 18 | HÔTEL-DIEU DE LÉVIS | 0 | 0 | 14 | 1.82 [1.08 - 3.08] | 0 | 0 |
| 20 | HÔPITAL DE CHICOUTIMI | 2 | 0.29 [0.07 - 1.16] | 8 | 1.16 [0.58 - 2.31] | 5 | 0.72 [0.30 1.74] |
| 21 | HÔPITAL SAINT-LUC DU CHUM | 13 | 1.28 [0.74 - 2.20] | 12 | 1.18 [0.67 - 2.08] | 23 | 2.26 [1.50 3.41] |
| 22 | HÔTEL-DIEU DU CHUM | 10 | 1.49 [0.80 2.77] | 6 | 0.89 [0.40 1.99] | 19 | 2.83 [1.81 - 4.44] |
| 24 | HÔPITAL DU SAINT-SACREMENT | 0 | 0 | 5 | 0.96 [0.40 2.30] | 2 | 0.38 [0.10 1.53] |
| 25 | HÔPITAL DU SACRÉ-COEUR DE MONTRÉAL | 25 | 1.71 [1.15 - 2.52] | 29 | 1.98 [1.37 - 2.85] | 8 | 0.55 [0.27 - 1.09] |
| 27 | PAVILLON CENTRE HOSPITALIER DE L'UNIVERSITÉ LAVAL | 7 | 0.6 [0.29 - 1.26] | 7 | 0.6 [0.29 - 1.26] | 0 | 0 |
| 28 | PAVILLON SAINT-FRANCOIS D'ASSISE | 5 | 0.56 [0.23 - 1.35] | 12 | 1.34 [0.76 - 2.37] | 5 | 0.56 [0.23 - 1.35] |
| 29 | HÔPITAL GÉNÉRAL DE MONTRÉAL | 23 | 3.22 [2.14 - 4.84] | 4 | 0.56 [0.21 - 1.49] | 21 | 2.94 [1.91 - 4.50] |
| 30 | HÔTEL-DIEU DE SHERBROOKE | 3 | 0.44 [0.14 - 1.35] | 7 | 1.02 [0.48 - 2.13] | 3 | 0.44 [0.14 - 1.35] |
| 31 | PAVILLON SAINTE-MARIE | 9 | 0.71 [0.37 - 1.37] | 14 | 1.11 [0.66 - 1.87] | 8 | 0.63 [0.32 - 1.26] |
| 33 | INSTITUT UNIVERSITAIRE DE CARDIOLOGIE ET DE PNEUMOLOGIE DE QUÉBEC | 3 | 0.3 [0.10 0.93] | 6 | 0.6 [0.27 - 1.34] | 18 | 1.81 [1.14 - 2.87] |
| 48 | CENTRE HOSPITALIER DE ST. MARY | 3 | 0.4 [0.13 - 1.23] | 16 | 2.12 [1.30 3.45] | 0 | 0 |
| 76 | HÔPITAL DE LACHINE | 0 | 0 | 4 | 2.24 [0.84 - 5.96] | 0 | 0 |
Tableau 10 – Incidence Rates of CRBSI and of BSIs Secondary to Urinary Tract and Pulmonary Infections per Facility and Percentile Ranking, for Non-Teaching Healthcare Facilities, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
| Facility | CRBSI | Urinairy tract | SSI | ||||
|---|---|---|---|---|---|---|---|
Cases (n) | Incidence rates | Cases (n) | Incidence rates | Cases (n) | Incidence rates | ||
| 9 | HÔPITAL DU HAUT-RICHELIEU | 5 | 0.57 [0.24 - 1.38] | 11 | 1.26 [0.70 2.28] | 1 | 0.11 [0.02 - 0.81] |
| 10 | HÔPITAL PIERRE-BOUCHER | 0 | 0 | 15 | 1.31 [0.79 - 2.17] | 2 | 0.17 [0.04 - 0.70] |
| 11 | HÔPITAL PIERRE-LE GARDEUR | 3 | 0.27 [0.09 - 0.82] | 13 | 1.15 [0.67 - 1.98] | 2 | 0.18 [0.04 - 0.71] |
| 14 | CENTRE HOSPITALIER RÉGIONAL DE LANAUDIÈRE | 4 | 0.39 [0.15 - 1.05] | 11 | 1.08 [0.60 1.96] | 6 | 0.59 [0.27 - 1.32] |
| 16 | HÔPITAL RÉGIONAL DE RIMOUSKI | 1 | 0.19 [0.03 - 1.33] | 6 | 1.13 [0.51 - 2.51] | 0 | 0 |
| 19 | HÔPITAL CITÉ DE LA SANTÉ | 10 | 0.58 [0.31 - 1.07] | 11 | 0.63 [0.35 - 1.14] | 6 | 0.35 [0.16 - 0.77] |
| 23 | HÔTEL-DIEU D'ARTHABASKA | 0 | 0 | 2 | 0.42 [0.10 1.66] | 3 | 0.62 [0.20 1.93] |
| 26 | HÔPITAL DE VERDUN | 13 | 1.58 [0.92 - 2.72] | 16 | 1.94 [1.19 - 3.17] | 3 | 0.36 [0.12 - 1.13] |
| 32 | CENTRE HOSPITALIER RÉGIONAL DU GRAND-PORTAGE | 1 | 0.4 [0.06 - 2.80] | 0 | 0 | 0 | 0 |
| 34 | HÔPITAL SANTA CABRINI | 2 | 0.2 [0.05 - 0.78] | 14 | 1.37 [0.81 - 2.32] | 3 | 0.29 [0.09 - 0.91] |
| 35 | HÔPITAL HONORÉ-MERCIER | 4 | 0.61 [0.23 - 1.63] | 7 | 1.07 [0.51 - 2.25] | 3 | 0.46 [0.15 - 1.43] |
| 36 | HÔPITAL GÉNÉRAL DU LAKESHORE | 1 | 0.13 [0.02 - 0.94] | 9 | 1.2 [0.62 - 2.30] | 1 | 0.13 [0.02 - 0.94] |
| 37 | HÔTEL-DIEU DE SOREL | 2 | 0.43 [0.11 - 1.70] | 8 | 1.7 [0.85 - 3.40] | 0 | 0 |
| 38 | HÔPITAL JEAN-TALON | 4 | 0.82 [0.31 - 2.18] | 4 | 0.82 [0.31 - 2.18] | 4 | 0.82 [0.31 - 2.18] |
| 39 | HÔPITAL DE GATINEAU | 0 | 0 | 10 | 1.64 [0.88 - 3.05] | 0 | 0 |
| 40 | HÔPITAL DE HULL | 4 | 0.6 [0.22 - 1.60] | 5 | 0.75 [0.31 - 1.80] | 2 | 0.3 [0.07 - 1.20] |
| 41 | HÔPITAL DU CENTRE-DE-LA-MAURICIE | 5 | 1.04 [0.43 - 2.49] | 7 | 1.45 [0.69 - 3.04] | 2 | 0.41 [0.10 1.66] |
| 42 | CENTRE HOSPITALIER ANNA-LABERGE | 1 | 0.14 [0.02 - 0.96] | 9 | 1.22 [0.63 - 2.34] | 2 | 0.27 [0.07 - 1.08] |
| 44 | HÔPITAL SAINTE-CROIX | 0 | 0 | 7 | 1.18 [0.56 - 2.48] | 3 | 0.51 [0.16 - 1.57] |
| 45 | HÔPITAL DE SAINT-EUSTACHE | 9 | 0.99 [0.52 - 1.91] | 3 | 0.33 [0.11 - 1.03] | 3 | 0.33 [0.11 - 1.03] |
| 46 | HÔPITAL DE GRANBY | 1 | 0.22 [0.03 - 1.55] | 8 | 1.74 [0.87 - 3.48] | 0 | 0 |
| 47 | HÔPITAL DE ROUYN-NORANDA | 0 | 0 | 2 | 0.86 [0.21 - 3.42] | 1 | 0.43 [0.06 - 3.04] |
| 49 | CSSS DE MEMPHREMAGOG | 0 | 0 | 0 | 0 | 0 | 0 |
| 51 | HÔPITAL DE MANIWAKI | 0 | 0 | 1 | 0.71 [0.10 5.04] | 0 | 0 |
| 52 | HÔPITAL D'AMOS | 0 | 0 | 0 | 0 | 0 | 0 |
| 53 | HÔPITAL DE CHANDLER | 0 | 0 | 0 | 0 | 0 | 0 |
| 56 | CENTRE DE SANTÉ ET DE SERVICES SOCIAUX D'ARGENTEUIL | 0 | 0 | 3 | 2.11 [0.68 - 6.55] | 0 | 0 |
| 58 | HÔPITAL DU SUROÎT | 1 | 0.17 [0.02 - 1.18] | 11 | 1.82 [1.01 - 3.29] | 1 | 0.17 [0.02 - 1.18] |
| 59 | HÔPITAL DE BAIE-SAINT-PAUL | 0 | 0 | 0 | 0 | 0 | 0 |
| 61 | HÔPITAL NOTRE-DAME-DE-FATIMA | 0 | 0 | 1 | 1.26 [0.18 - 8.94] | 0 | 0 |
| 63 | HÔPITAL DE SAINT-GEORGES | 0 | 0 | 0 | 0 | 0 | 0 |
| 64 | HÔPITAL LE ROYER | 1 | 0.47 [0.07 - 3.33] | 3 | 1.41 [0.45 - 4.36] | 0 | 0 |
| 65 | HÔPITAL ET CLSC DE VAL-D'OR | 0 | 0 | 0 | 0 | 0 | 0 |
| 67 | HÔPITAL ET CENTRE DE RÉADAPTATION DE JONQUIÈRE | 0 | 0 | 3 | 0.78 [0.25 - 2.41] | 0 | 0 |
| 70 | CENTRE DE SOINS DE COURTE DURÉE LA SARRE | 0 | 0 | 0 | 0 | 0 | 0 |
| 71 | HÔPITAL DE MATANE | 0 | 0 | 1 | 0.85 [0.12 - 6.04] | 0 | 0 |
| 72 | HÔPITAL ET CENTRE D'HÉBERGEMENT DE SEPT-ÎLES | 1 | 0.48 [0.07 - 3.39] | 0 | 0 | 0 | 0 |
| 74 | HÔPITAL DE DOLBEAU-MISTASSINI | 0 | 0 | 0 | 0 | 0 | 0 |
| 75 | CSSS DU GRANIT | 0 | 0 | 1 | 1.01 [0.14 - 7.14] | 0 | 0 |
| 77 | HÔPITAL D'AMQUI | 0 | 0 | 0 | 0 | 0 | 0 |
| 80 | HÔPITAL FLEURY | 4 | 1.01 [0.38 - 2.68] | 7 | 1.76 [0.84 - 3.69] | 4 | 1.01 [0.38 - 2.68] |
| 81 | HÔPITAL DE MONT-LAURIER | 1 | 0.56 [0.08 - 4.00] | 1 | 0.56 [0.08 - 4.00] | 0 | 0 |
| 82 | PAVILLON SAINTE-FAMILLE | 1 | 1.5 [0.21 - 10.64] | 0 | 0 | 0 | 0 |
| 83 | HÔPITAL DE LASALLE | 0 | 0 | 0 | 0 | 0 | 0 |
| 84 | HÔPITAL DE NOTRE-DAME-DU-LAC | 0 | 0 | 0 | 0 | 0 | 0 |
| 85 | CENTRE DE SANTÉ ET DE SERVICES SOCIAUX DU HAUT-SAINT-MAURICE | 0 | 0 | 0 | 0 | 1 | 1.32 [0.19 - 9.34] |
| 86 | HÔPITAL DE LA MALBAIE | 0 | 0 | 0 | 0 | 0 | 0 |
| 88 | HÔPITAL. CLSC ET CENTRE D'HÉBERGEMENT DE ROBERVAL | 0 | 0 | 2 | 0.84 [0.21 - 3.35] | 0 | 0 |
| 89 | HÔPITAL DE MONTMAGNY | 0 | 0 | 1 | 0.59 [0.08 - 4.18] | 1 | 0.59 [0.08 - 4.18] |
| 91 | HÔPITAL HÔTEL-DIEU DE GASPÉ | 0 | 0 | 1 | 0.92 [0.13 - 6.57] | 0 | 0 |
| 95 | HÔPITAL DU PONTIAC | 0 | 0 | 0 | 0 | 0 | 0 |
| 96 | CENTRE DE SANTÉ DE CHIBOUGAMAU | 0 | 0 | 0 | 0 | 0 | 0 |
| 97 | HÔPITAL DE MARIA | 0 | 0 | 1 | 0.57 [0.08 - 4.01] | 1 | 0.57 [0.08 - 4.01] |
| 99 | HÔPITAL BROME-MISSISQUOI-PERKINS | 1 | 0.4 [0.06 - 2.85] | 4 | 1.61 [0.60 4.28] | 0 | 0 |
| 100 | HÔPITAL DE LA BAIE | 0 | 0 | 1 | 0.72 [0.10 5.09] | 0 | 0 |
| 101 | HÔPITAL RÉGIONAL DE SAINT-JÉRÔME | 14 | 1.29 [0.77 - 2.19] | 8 | 0.74 [0.37 - 1.48] | 11 | 1.02 [0.56 - 1.84] |
| 103 | HÔPITAL LAURENTIEN | 2 | 0.64 [0.16 - 2.56] | 3 | 0.96 [0.31 - 2.97] | 0 | 0 |
| 107 | HÔPITAL DE L'ARCHIPEL | 1 | 1.28 [0.18 - 9.08] | 0 | 0 | 1 | 1.28 [0.18 - 9.08] |
| 109 | HÔPITAL DE SAINTE-ANNE-DES-MONTS | 0 | 0 | 0 | 0 | 0 | 0 |
| 111 | HÔPITAL DE PAPINEAU | 0 | 0 | 2 | 1 [0.25 - 3.98] | 0 | 0 |
| 112 | HÔPITAL D'ALMA | 1 | 0.31 [0.04 - 2.20] | 1 | 0.31 [0.04 - 2.20] | 0 | 0 |
| 113 | HÔPITAL DE THETFORD MINES | 0 | 0 | 3 | 1.34 [0.43 - 4.16] | 0 | 0 |
| 130 | HÔPITAL BARRIE MÉMORIAL | 0 | 0 | 0 | 0 | 0 | 0 |
Abbreviations
95% CI: 95% confidence interval
BSI: bloodstream infection
CoNS: coagulase-negative Staphylococcus
CRBSI: catheter-related bloodstream infection
HD: hemodialysis
ICU: intensive care unit
MBI: mucosal barrier injury
Non-CRBSI: non-catheter-related primary bloodstream infection
SSI: surgical site infection
Author
Comité de surveillance provinciale des infections nosocomiales (SPIN) – bactériémies panhospitalières
Editorial Committee
Élise Fortin, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Muleka Ngenda-Muadi, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Isabelle Rocher, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Marc-André Smith, Hôpital du Sacré-Cœur de Montréal
Claude Tremblay, Centre hospitalier universitaire de Québec de Québec – Université Laval
Mélissa Trudeau, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Jasmin Villeneuve, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec


![Figure 1 – BSI Incidence Rate for Each Type of Infection, by Type of Healthcare Facility, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI]) Figure 1 – BSI Incidence Rate for Each Type of Infection, by Type of Healthcare Facility, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])](/sites/default/files/images/maladies-infectieuses/spin/bactot/2017/en/figure1.png)
![Figure 2 – BSI Incidence Rate in ICUs, For Each Type of Infection, by Type of Healthcare Facility and Type of ICU, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI]) Figure 2 – BSI Incidence Rate in ICUs, For Each Type of Infection, by Type of Healthcare Facility and Type of ICU, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])](/sites/default/files/images/maladies-infectieuses/spin/bactot/2017/en/figure2.png)
![Figure 3 – BSI Incidence Rate in Non-ICU Units, for Each Type of Infection, by Type of Healthcare Facility, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI]) Figure 3 – BSI Incidence Rate in Non-ICU Units, for Each Type of Infection, by Type of Healthcare Facility, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])](/sites/default/files/images/maladies-infectieuses/spin/bactot/2017/en/figure3.png)
![Figure 4 – Evolution of BSI Incidence Rates, by Type of Infection, in Facilities that Previously participated in Surveillance (N = 89), Québec, 2012–2016 and 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI]) Figure 4 – Evolution of BSI Incidence Rates, by Type of Infection, in Facilities that Previously participated in Surveillance (N = 89), Québec, 2012–2016 and 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])](/sites/default/files/images/maladies-infectieuses/spin/bactot/2017/en/figure4.png)