Central Line–Associated Bloodstream Infections in Intensive Care Units Surveillance results: 2016-2017

From April 1st, 2016, to March 31st, 2017, 69 intensive care units (ICUs) took part in surveillance of central line–associated bloodstream infections (CLABSIs), for a combined total of 135,114 catheter days (Table 1). Participating ICUs report 133 CLABSIs in 125 patients. Incidence rates are 0.91 per 1,000 catheter days in coronary ICUs, 0.62 in teaching adult ICUs, 0.46 in non-teaching adult ICUs, 2.16 in pediatric ICUs and 2.78 in neonatal ICUs. The incidence rates in 2016–2017 are lower compared to 2012–2016 in neonatal ICUs while they remain statistically stable in other ICU types. Compared to 2015-2016, one adult non-teaching ICUs with less than 10 beds has stopped participating to surveillance while two coronary ICUs and one adult teaching joined the surveillance. Data were extracted on May 5th, 2017.
Update: October 5, 2017
Version française
Table 1 – Evolution of the Participation of ICUs in the Surveillance of CLABSIs, Québec, 2012–2013 to 2016–2017
2012-2013 | 2013-2014 | 2014-2015 | 2015-2016 | 2016-2017 | |
|---|---|---|---|---|---|
| Participating ICUs (N) | 65 | 66 | 70 | 67 | 69 |
| Patient days (N) | 293,617 | 303,093 | 308,795 | 299,341 | 314,806 |
| Catheter days (N) | 127,322 | 129,982 | 131,677 | 128,123 | 135,114 |
| CLABSIs (cat. 1a and 1b, N) | 195 | 170 | 118 | 151 | 133 |
| Infected patients (N) | 191 | 157 | 115 | 140 | 125 |
Incidence rates
In 2016–2017, incidence rates are 0.91 per 1,000 catheter days in coronary ICUs, 0.62 in teaching adult ICUs, 0.46 in non-teaching adult ICUs, 2.16 in pediatric ICUs and 2.78 in neonatal ICUs. The lowest pooled mean rate is thus found in adult non-teaching ICUs (Table 2). The CLABSI incidence rate is highest in neonatal and pediatric ICUs, and these rates are significantly higher than that of adult ICUs (p < 0.05). Even though the main case definition excludes infections with a mucosal barrier injury, Table 2 also presents rates including these cases, to allow comparisons with American incidence rates. In neonatal ICUs, rates tend to increase as birth weight decreases (Table 3).
Table 2 – CLABSI Incidence Rate and Catheter Utilization Ratio, by Type of Healthcare Facility and Type of ICU, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days [95% CI])
Type of ICU | ICUs (N) | Incidence rate | Incidence rate (including mucosal barrier injuries) | Utilization ratio |
|---|---|---|---|---|
| Coronary | 3 | 0.91 [0.23 ;3.66] | 0.91 [0.23 ;3.66] | 0.24 |
| Adult, teaching | 26 | 0.62 [0.47 ;0.82] | 0.64 [0.49 ;0.85] | 0.63 |
| Adult, non-teaching | 29 | 0.46 [0.27 ;0.80] | 0.50 [0.30 ;0.84] | 0.32 |
| Pediatric | 4 | 2.16 [1.38 ;3.39] | 2.39 [1.56 ;3.67] | 0.67 |
| Neonatal | 7 | 2.78 [2.11 ;3.65] | 2.83 [2.16 ;3.71] | 0.23 |
95% CI: 95% confidence interval.
Table 3 – CLABSI Incidence Rate in Neonatal ICUs, by Birth Weight Category, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days [95% CI])
Birth weight category (grams) | Number of cases | Incidence Rates |
|---|---|---|
≤750 | 20 | 5.76 [3.72 ; 8.93] |
751-1,000 | 12 | 3.04 [1.73 ; 5.36] |
1,001-1,500 | 11 | 2.95 [1.63 ; 5.33] |
1,501-2,500 | 3 | 0.92 [0.30 ; 2.84] |
>2,500 | 5 | 1.26 [0.53 ; 3.04] |
Total | 51 | 2.78 [2.11 ; 3.65] |
Incidence rates trends
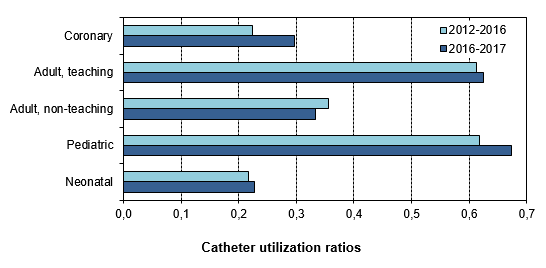
In 2016–2017, compared to the previous four years (Figure 1), CLABSI incidence rates declined significantly in neonatal ICUs (p < 0.05), but remained stable (p > 0.05) in adult teaching ICUs, adult non-teaching ICUs, pediatric ICUs and coronary ICUs.
Figure 1 – Evolution of CLABSI Incidence Rates, by Type of Healthcare Facility and Type of ICU, in ICUs that previously participated in SPIN (N = 67), Québec, 2012–2016 and 2016–2017 (Incidence Rate per 1,000 Catheter days [95% CI])
Figure 2 – Evolution of Catheter Utilization Ratios, by Type of Healthcare Facility and Type of ICU, in ICUs that previously participated in SPIN (N = 67), Québec, 2012–2016 and 2016–2017
Description of cases
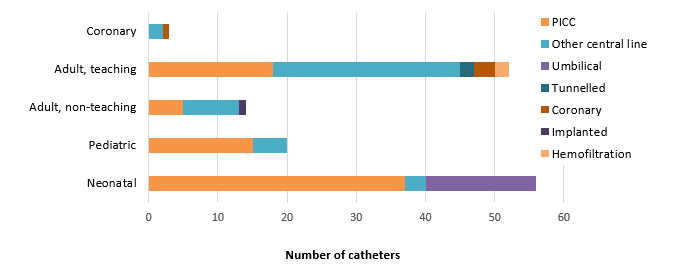
Patients who developed a CLABSI are aged between 0 and 94 years, with a median age of 66 years old in the adult ICUs, 0.5 years old in pediatric ICUs and of a little less than one month old in neonatal ICUs. In adult ICUs, the central lines most frequently associated with bloodstream infections are the 'other' central venous catheters (CVCs) that include central lines previously named 'regular' CVCs, followed by peripherally inserted central catheters (PICCs) (Figure 3). In neonatal ICUs, PICCs are the most frequently associated with CLABSI, followed by umbilical catheters.
Figure 3 – Type of Central Line Used in CLABSI Cases, by Type of Healthcare Facility and Type of ICU, Québec, 2016–2017 (N)
NB: More than one central line may be reported in any given case of CLABSI, which explains why the total number of central lines is higher than the total number of CLABSIs presented earlier in this paper.
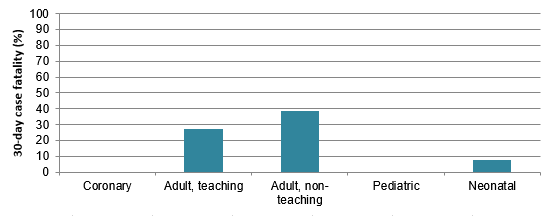
In 2016–2017, 17 % of CLABSI cases died within 30 days after bacteremia onset (Table 4). Case fatality is 0 % in coronary ICUs (Table 4) but the number of cases is very small. The overall case fatality of 17 % is not a significant increase compared to the case fatality of 13 % observed in 2015–2016 (p > 0.05).
Figure 4 – 30-Day Case Fatality, by Type of Healthcare Facility and Type of ICU, Québec, 2016–2017 (%)
Table 4 – 30-Day Case Fatality, by Type of Healthcare Facility and Type of ICU, Québec, 2016–2017 (N, %)
| Type of ICU | CLABSIS (N) | Death within 10 days | Death within 30 days | ||
|---|---|---|---|---|---|
N | % | N | % | ||
| Coronary | 2 | 0 | 0 | 0 | 0 |
| Adult, teaching | 48 | 9 | 19 | 13 | 27 |
| Adult, non-teaching | 13 | 1 | 8 | 5 | 38 |
| Pediatric | 19 | 0 | 0 | 0 | 0 |
| Neonatal | 51 | 3 | 6 | 4 | 8 |
| Total | 133 | 13 | 10 | 22 | 17 |
Microbiology
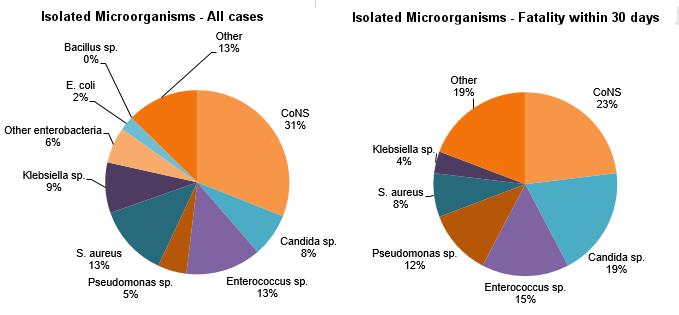
Figure 5 shows that the microorganisms most frequently isolated in reported CLABSI cases are coagulase-negative staphylococci (CoNS, 31 %), followed by Enterococcus sp. (13 %) then S. aureus (13 %). However, CoNS and Candida sp. are present in almost two thirds of cases resulting in death (57 %).
Figure 5 – Categories of Isolated Microorganisms in All Cases (N = 158) and Cases of Mortality Within 30 Days (N = 26), Québec, 2016–2017 (%)
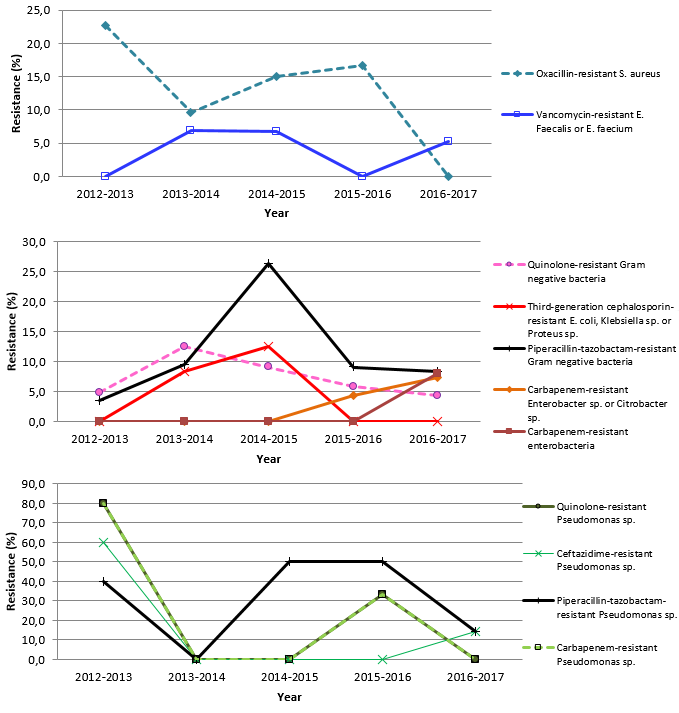
In 2016–2017, no S. aureus strains are resistant to oxacillin and one Enterococcus faecium resistant to vancomycin is reported (Table 5), for a global resistance proportion of 5 % among all E. faecium and E. faecalis. Two carbapenem-resistant enterobacteria are reported: one Klebsiella oxytoca and one Citrobacter freundii (Figure 6). Please note that the second graph in Figure 6 presents data that exclude Pseudomonas sp.
Table 5 – Percentage of Strains Tested and Percentage of Resistance to Antibiotics for Certain Isolated Microorganisms, Québec, 2016–2017 (N, %)
| Microorganism | Antibiotic | Isolated | Tested | Resistant | ||
|---|---|---|---|---|---|---|
N | N | % | N | % | ||
| Staphylococcus aureus | Oxacillin | 20 | 20 | 100 | 0 | 0 |
| Enterococcus faecium | Vancomycin | 7 | 7 | 100 | 1 | 14.3 |
| Enterococcus faecalis | Vancomycin | 12 | 12 | 100 | 0 | 0 |
| Klebsiella sp. | CSE 4 | 14 | 10 | 71.4 | 0 | 0 |
| Imipenem ou meropenem | 14 | 11 | 78.6 | 1 | 9.1 | |
| Multiresistant 1 | 14 | 12 | 85.7 | 0 | 0 | |
| Escherichia coli | CSE 4 | 4 | 4 | 100 | 0 | 0 |
| Fluoroquinolones 3 | 4 | 4 | 100 | 0 | 0 | |
| Imipenem ou meropenem | 4 | 4 | 100 | 0 | 0 | |
| Multiresistant 1 | 4 | 4 | 100 | 0 | 0 | |
| Enterobacter sp. | CSE 4 | 5 | 3 | 60 | 1 | 33.3 |
| Imipenem ou meropenem | 5 | 5 | 100 | 0 | 0 | |
| Multiresistant 1 | 5 | 3 | 60 | 0 | 0 | |
| Pseudomonas sp. | Amikacin, gentamicin or tobramycin | 8 | 7 | 87.5 | 0 | 0 |
| CSE 2 | 8 | 7 | 87.5 | 1 | 14.3 | |
| Fluoroquinolones 2 | 8 | 7 | 87.5 | 0 | 0 | |
| Imipenem ou meropenem | 8 | 7 | 87.5 | 0 | 0 | |
| Piperacillin/tazobactam | 8 | 7 | 87.5 | 1 | 14.3 | |
| Multiresistant 2 | 8 | 7 | 87.5 | 0 | 0 | |
| Acinetobacter sp. | Imipenem ou meropenem | 1 | 1 | 100 | 0 | 0 |
| Multiresistant 3 | 1 | 0 | 0 | - | - | |
CSE 2: cefepime or ceftazidime;
CSE 4: cefepime, cefotaxime, ceftazidime or ceftriaxone;
Fluoroquinolones 2: ciprofloxacin or levofloxacin;
Fluoroquinolones 3: ciprofloxacin, levofloxacin or moxifloxacin;
Multiresistant 1: intermediate or resistant to an agent in three of the following five categories: cephalosporins 4, fluoroquinolones 3, aminoglycosides, carbapenems, piperacillin or piperacillin/tazobactam.
Multiresistant 2: intermediate or resistant to an agent in three of the following five categories: cephalosporins 2, fluoroquinolones 2, aminoglycosides, carbapenems, piperacillin or piperacillin/tazobactam.
Multiresistant 3: intermediate or resistant to an agent in three of the following six categories: cephalosporins 2, fluoroquinolones 2, aminoglycosides, carbapenems, piperacillin or piperacillin/tazobactam, ampicillin/sulbactam.
Figure 6 – Evolution of Antibiotic Resistance in Gram-Positive Bacteria, Gram-Negative Bacteria and Pseudomonas sp., Québec, 2012–2013 to 2016–2017 (%)
Results per ICU
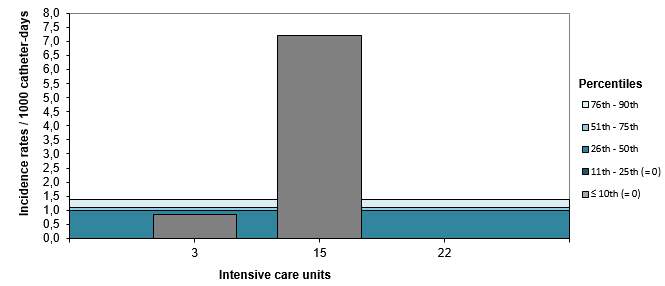
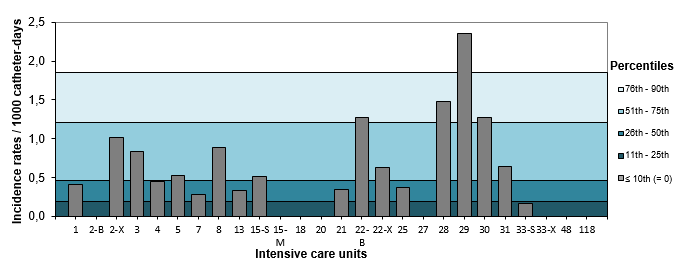
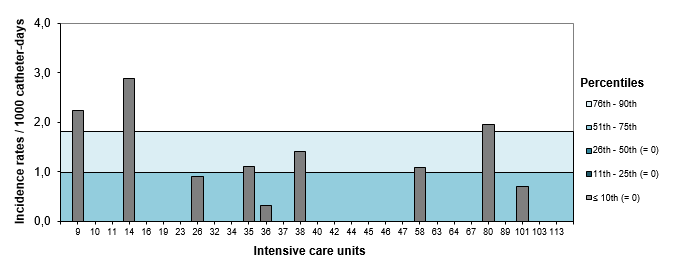
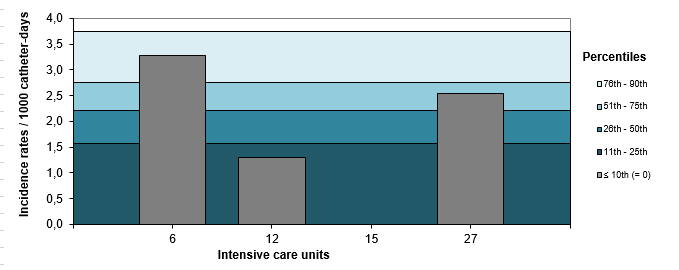
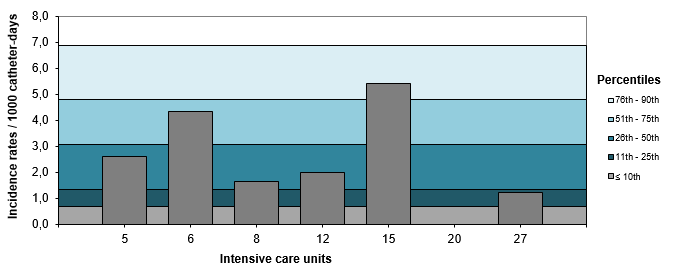
In 2016–2017, one coronary ICU (33 % of ICUs), one adult teaching ICU (4 % of ICUs) and three adult non-teaching ICUs (10 % of ICUs) remain below the 90th percentile of 2012–2013 to 2015–2016 rates for their ICU type (Figures 7, 8 and 9). No pediatric or neonatal ICU ranks above the 90th percentile in their respective units type (figures 10 and 11). Tables 6 and 7 present the numerical values that correspond to the rates displayed in Figures 7 through 11. Tables 8 and 9 show the catheter utilization rates for each ICU.
Figure 7 – CLABSI Incidence Rate per ICU (2016–2017) and Percentile Ranking (2012–2013 to 2015–2016), Coronary ICUs, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days)
Figure 8 – CLABSI Incidence Rate per ICU (2016–2017) and Percentile Ranking (2012–2013 to 2015–2016), Teaching Adult ICUs, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days)
Figure 9 – CLABSI Incidence Rate per ICU (2016–2017) and Percentile Ranking (2012–2013 to 2015–2016), Non-Teaching Adult ICUs, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days)
Figure 10 – CLABSI Incidence Rate (2015–2016) and Percentile Ranking (2012–2013 to 2015–2016) per ICU, Pediatric ICUs, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days)
Figure 11 – CLABSI Incidence Rate (2016–2017) and Percentile Ranking (2012–2013 to 2015–2016), per ICU, Neonatal ICUs, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days)
NB for Figures 7 to 11: In healthcare facilities with more than one type of ICU: S = surgical, M = medical, X = mixed and B = burn trauma.
Table 6 – CLABSI Incidence Rate per ICU, Distribution of CLABSI rates for 2012–2016, by ICU Types, for Teaching Healthcare Facilities, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days)
| Facility | Adult, teaching* | Coronary | Pediatric | Neonatal | |
|---|---|---|---|---|---|
| 1 | HÔPITAL CHARLES LEMOYNE | 0.41 |
|
|
|
| 2 | HÔPITAL DE L'ENFANT-JÉSUS | 0.00-B |
|
|
|
| 2 | HÔPITAL DE L'ENFANT-JÉSUS | 1.01-X |
|
|
|
| 3 | GLEN - ROYAL VICTORIA | 0.83 | 0.86 |
|
|
| 4 | HÔPITAL NOTRE-DAME DU CHUM | 0.45 |
|
|
|
| 5 | HÔPITAL GÉNÉRAL JUIF | 0.53 |
|
| 2.63 |
| 6 | GLEN - ENFANTS | 2.74 | 4.33 | ||
| 7 | PAVILLON L'HÔTEL-DIEU DE QUÉBEC | 0.28 |
|
| |
| 8 | PAVILLON MAISONNEUVE/PAVILLON MARCEL-LAMOUREUX | 0.89 |
| 1.63 | |
| 12 | CENTRE HOSPITALIER UNIVERSITAIRE SAINTE-JUSTINE | 2.37 | 1.99 | ||
| 13 | INSTITUT DE CARDIOLOGIE DE MONTRÉAL | 0.34 |
|
|
|
| 15 | HÔPITAL FLEURIMONT | 0.52-C | 7.19 | 0 | 5.42 |
| 15 | HÔPITAL FLEURIMONT | 0.00-M |
|
|
|
| 18 | HÔTEL-DIEU DE LÉVIS | 0 |
|
|
|
| 20 | HÔPITAL DE CHICOUTIMI | 0 |
|
| 0 |
| 21 | HÔPITAL SAINT-LUC DU CHUM | 0.34 |
|
|
|
| 22 | HÔTEL-DIEU DU CHUM | 1.28-B | 0 |
|
|
| 22 | HÔTEL-DIEU DU CHUM | 0.62-X |
|
|
|
| 25 | HÔPITAL DU SACRÉ-COEUR DE MONTRÉAL | 0.37 |
|
|
|
| 27 | PAVILLON CENTRE HOSPITALIER DE L'UNIVERSITÉ LAVAL | 0 |
| 0 | 1.23 |
| 28 | PAVILLON SAINT-FRANÇOIS D'ASSISE | 1.48 |
|
|
|
| 29 | HÔPITAL GÉNÉRAL DE MONTRÉAL | 2.36 |
|
|
|
| 30 | HÔTEL-DIEU DE SHERBROOKE | 1.28 |
|
|
|
| 31 | PAVILLON SAINTE-MARIE | 0.64 |
| ||
| 33 | INSTITUT UNIVERSITAIRE DE CARDIOLOGIE ET DE PNEUMOLOGIE DE QUÉBEC | 0.17-C |
| ||
| 33 | INSTITUT UNIVERSITAIRE DE CARDIOLOGIE ET DE PNEUMOLOGIE DE QUÉBEC | 0.00-X |
| ||
| 48 | CENTRE HOSPITALIER DE ST. MARY | 0 |
| ||
| 118 | HÔPITAL NEUROLOGIQUE DE MONTRÉAL | 0 |
| ||
| 2012-2016 percentile ranking | 10th | 0 | 0 | 0 | 0.68 |
| 25th | 0.19 | 0 | 1.56 | 1.36 | |
| 50th | 0.47 | 0.98 | 2.21 | 3.09 | |
| 75th | 1.21 | 1.11 | 2.75 | 4.82 | |
| 90th | 1.85 | 1.39 | 3.73 | 6.87 | |
* In healthcare facilities with more than one type of adult ICU: S = surgical, M = medical, X = mixed and B = burn trauma.
Table 7 – CLABSI Incidence Rate per ICU, Distribution of CLABSI rates for 2012–2016, by ICU Types, for Non-teaching Healthcare Facilities, Québec, 2016–2017 (Incidence Rate per 1,000 Catheter days)
| Facility | Adult, non-teaching | |
|---|---|---|
| 9 | HÔPITAL DU HAUT-RICHELIEU | 2.23 |
| 10 | HÔPITAL PIERRE-BOUCHER | 0 |
| 11 | HÔPITAL PIERRE-LE GARDEUR | 0 |
| 14 | CENTRE HOSPITALIER RÉGIONAL DE LANAUDIÈRE | 2.88 |
| 16 | HÔPITAL RÉGIONAL DE RIMOUSKI | 0 |
| 19 | HÔPITAL CITÉ DE LA SANTÉ | 0 |
| 23 | HÔTEL-DIEU D'ARTHABASKA | 0 |
| 26 | HÔPITAL DE VERDUN | 0.90 |
| 32 | CENTRE HOSPITALIER RÉGIONAL DU GRAND-PORTAGE | 0 |
| 34 | HÔPITAL SANTA CABRINI | 0 |
| 35 | HÔPITAL HONORÉ-MERCIER | 1.10 |
| 36 | HÔPITAL GÉNÉRAL DU LAKESHORE | 0.32 |
| 37 | HÔTEL-DIEU DE SOREL | 0 |
| 38 | HÔPITAL JEAN-TALON | 1.42 |
| 40 | HÔPITAL DE HULL | 0 |
| 42 | CENTRE HOSPITALIER ANNA-LABERGE | 0 |
| 44 | HÔPITAL SAINTE-CROIX | 0 |
| 45 | HÔPITAL DE SAINT-EUSTACHE | 0 |
| 46 | HÔPITAL DE GRANBY | 0 |
| 47 | HÔPITAL DE ROUYN-NORANDA | 0 |
| 58 | HÔPITAL DU SUROÎT | 1.09 |
| 63 | HÔPITAL DE SAINT-GEORGES | 0 |
| 64 | HÔPITAL LE ROYER | 0 |
| 67 | HÔPITAL ET CENTRE DE RÉADAPTATION DE JONQUIÈRE | 0 |
| 80 | HÔPITAL FLEURY | 1.95 |
| 89 | HÔPITAL DE MONTMAGNY | 0 |
| 101 | HÔPITAL RÉGIONAL DE SAINT-JÉRÔME | 0.70 |
| 103 | HÔPITAL LAURENTIEN | 0 |
| 113 | HÔPITAL DE THETFORD MINES | 0 |
| 2012-2016 percentile ranking | 10th | 0 |
| 25th | 0 | |
| 50th | 0 | |
| 75th | 1.00 | |
| 90th | 1.82 | |
Table 8 – Catheter Utilization Ratio per ICU, Distribution of Ratios for 2012–2016, by ICU Types, for Teaching Healthcare Facilities, Québec, 2016–2017
| Facility | Adult, teaching* | Coronary | Pediatric | Neonatal | |
|---|---|---|---|---|---|
| 1 | HÔPITAL CHARLES LEMOYNE | 0.50 |
|
|
|
| 2 | HÔPITAL DE L'ENFANT-JÉSUS | 0.29-B |
|
|
|
| 2 | HÔPITAL DE L'ENFANT-JÉSUS | 0.44-X |
|
|
|
| 3 | GLEN - ROYAL VICTORIA | 0.77 | 0.27 |
|
|
| 4 | HÔPITAL NOTRE-DAME DU CHUM | 0.98 |
|
|
|
| 5 | HÔPITAL GÉNÉRAL JUIF | 0.86 |
|
| 0.22 |
| 6 | GLEN - ENFANTS | 0.92 | 0.31 | ||
| 7 | PAVILLON L'HÔTEL-DIEU DE QUÉBEC | 0.70 |
|
|
|
| 8 | PAVILLON MAISONNEUVE/PAVILLON MARCEL-LAMOUREUX | 0.49 |
|
| 0.10 |
| 12 | CENTRE HOSPITALIER UNIVERSITAIRE SAINTE-JUSTINE | 0.70 | 0.26 | ||
| 13 | INSTITUT DE CARDIOLOGIE DE MONTRÉAL | 1 |
|
|
|
| 15 | HÔPITAL FLEURIMONT | 0.49-C | 0.06 | 0.18 | 0.21 |
| 15 | HÔPITAL FLEURIMONT | 0.34-M |
|
|
|
| 18 | HÔTEL-DIEU DE LÉVIS | 0.34 |
|
|
|
| 20 | HÔPITAL DE CHICOUTIMI | 0.82 |
|
| 0.17 |
| 21 | HÔPITAL SAINT-LUC DU CHUM | 0.85 |
|
|
|
| 22 | HÔTEL-DIEU DU CHUM | 0.65-B | 0 |
|
|
| 22 | HÔTEL-DIEU DU CHUM | 1.06-X |
|
|
|
| 25 | HÔPITAL DU SACRÉ-COEUR DE MONTRÉAL | 0.58 |
|
|
|
| 27 | PAVILLON CENTRE HOSPITALIER DE L'UNIVERSITÉ LAVAL | 0.10 |
| 0.46 | 0.17 |
| 28 | PAVILLON SAINT-FRANÇOIS D'ASSISE | 0.36 |
|
|
|
| 29 | HÔPITAL GÉNÉRAL DE MONTRÉAL | 0.74 |
|
|
|
| 30 | HÔTEL-DIEU DE SHERBROOKE | 0.22 |
|
|
|
| 31 | PAVILLON SAINTE-MARIE | 0.61 |
|
|
|
| 33 | INSTITUT UNIVERSITAIRE DE CARDIOLOGIE ET DE PNEUMOLOGIE DE QUÉBEC | 0.93-C |
|
|
|
| 33 | INSTITUT UNIVERSITAIRE DE CARDIOLOGIE ET DE PNEUMOLOGIE DE QUÉBEC | 0.47-X |
|
|
|
| 48 | CENTRE HOSPITALIER DE ST. MARY | 0.40 |
|
|
|
| 118 | HÔPITAL NEUROLOGIQUE DE MONTRÉAL | 0.19 |
|
|
|
| 2012-2016 percentile ranking | 10th | 0.30 | 0.15 | 0.17 | 0.02 |
| 25th | 0.46 | 0.16 | 0.4 | 0.14 | |
| 50th | 0.64 | 0.32 | 0.55 | 0.20 | |
| 75th | 0.87 | 0.37 | 0.69 | 0.24 | |
| 90th | 0.97 | 0.37 | 0.73 | 0.36 | |
* In healthcare facilities with more than one type of adult ICU: S = surgical, M = medical, X = mixed and B = burn trauma.
Table 9 – Catheter Utilization Ratio per ICU, Breakdown for 2012–2016, by ICU Types, for Non-teaching Healthcare Facilities, Québec, 2016–2017
| Facility | Adult, non-teaching | |
|---|---|---|
| 9 | HÔPITAL DU HAUT-RICHELIEU | 0.25 |
| 10 | HÔPITAL PIERRE-BOUCHER | 0.37 |
| 11 | HÔPITAL PIERRE-LE GARDEUR | 0.58 |
| 14 | CENTRE HOSPITALIER RÉGIONAL DE LANAUDIÈRE | 0.12 |
| 16 | HÔPITAL RÉGIONAL DE RIMOUSKI | 0.22 |
| 19 | HÔPITAL CITÉ DE LA SANTÉ | 0.34 |
| 23 | HÔTEL-DIEU D'ARTHABASKA | 0.12 |
| 26 | HÔPITAL DE VERDUN | 0.58 |
| 32 | CENTRE HOSPITALIER RÉGIONAL DU GRAND-PORTAGE | 0.28 |
| 34 | HÔPITAL SANTA CABRINI | 0.30 |
| 35 | HÔPITAL HONORÉ-MERCIER | 0.28 |
| 36 | HÔPITAL GÉNÉRAL DU LAKESHORE | 0.82 |
| 37 | HÔTEL-DIEU DE SOREL | 0.24 |
| 38 | HÔPITAL JEAN-TALON | 0.38 |
| 40 | HÔPITAL DE HULL | 0.71 |
| 42 | CENTRE HOSPITALIER ANNA-LABERGE | 0.43 |
| 44 | HÔPITAL SAINTE-CROIX | 0.11 |
| 45 | HÔPITAL DE SAINT-EUSTACHE | 0.23 |
| 46 | HÔPITAL DE GRANBY | 0.19 |
| 47 | HÔPITAL DE ROUYN-NORANDA | 0.11 |
| 58 | HÔPITAL DU SUROÎT | 0.34 |
| 63 | HÔPITAL DE SAINT-GEORGES | 0.33 |
| 64 | HÔPITAL LE ROYER | 0.20 |
| 67 | HÔPITAL ET CENTRE DE RÉADAPTATION DE JONQUIÈRE | 0.10 |
| 80 | HÔPITAL FLEURY | 0.19 |
| 89 | HÔPITAL DE MONTMAGNY | 0.03 |
| 101 | HÔPITAL RÉGIONAL DE SAINT-JÉRÔME | 0.37 |
| 103 | HÔPITAL LAURENTIEN | 0.07 |
| 113 | HÔPITAL DE THETFORD MINES | 0.08 |
| 2012-2016 percentile ranking | 10th | 0.15 |
| 25th | 0.22 | |
| 50th | 0.31 | |
| 75th | 0.44 | |
| 90th | 0.60 | |
Author
Comité de surveillance provinciale des infections nosocomiales (SPIN) – bactériémies sur cathéters centraux aux soins intensifs
Editorial Committee
Élise Fortin, Direction des risques biologiques et de la santé au travail. Institut national de santé publique du Québec
Muleka Ngenda-Muadi, Direction des risques biologiques et de la santé au travail. Institut national de santé publique du Québec
Caroline Quach, Centre universitaire de santé McGill. Hôpital de Montréal pour enfants
Isabelle Rocher, Direction des risques biologiques et de la santé au travail. Institut national de santé publique du Québec
Claude Tremblay, Centre hospitalier universitaire de Québec de Québec – Université Laval
Mélissa Trudeau, Direction des risques biologiques et de la santé au travail. Institut national de santé publique du Québec
Jasmin Villeneuve, Direction des risques biologiques et de la santé au travail. Institut national de santé publique du Québec


![Figure 1 – Evolution of CLABSI Incidence Rates, by Type of Healthcare Facility and Type of ICU, in ICUs that previously participated in SPIN (N = 67), Québec, 2012–2016 and 2016–2017 (Incidence Rate per 1,000 Catheter days [95% CI]) Figure 1 – Evolution of CLABSI Incidence Rates, by Type of Healthcare Facility and Type of ICU, in ICUs that previously participated in SPIN (N = 67), Québec, 2012–2016 and 2016–2017 (Incidence Rate per 1,000 Catheter days [95% CI])](/sites/default/files/images/maladies-infectieuses/spin/bacc/2017/en/figure1.png)