Carbapenemase-Producing Gram Negative Bacilli Infections Surveillance results: 2016-2017
 Carbapenemase-Producing Gram Negative Bacilli Infections
Carbapenemase-Producing Gram Negative Bacilli Infections
Surveillance results: 2016-2017
From April 1st, 2016, to March 31st, 2017, 82 healthcare facilities took part in the surveillance of carbapenemase-producing Gram negative bacilli (CPGNB) infections, for a total of 4,448,999 patient days (Table 1). These facilities reported 17 healthcare-associated CPGNB (HA-CPGNB) infections among patients who acquired their strain during a current or previous hospitalization (categories 1a and 1b). The incidence rate of HA-CPGNB infection was 0.04 per 10,000 patient days. The acquisition rate of HA-CPGNB colonization was 0.57 per 10,000 patient days. Eight infections were observed among healthcare facilities that joined the surveillance this year. Two teaching and one non-teaching facilities discontinued their participation this year whereas three teaching and nine non-teaching facilities joined the program. Data were extracted on June 1st, 2017.
Update: October 5, 2017
Version française
Table 1 – Participation of Healthcare Facilities in the Surveillance of CPGNB Infections, Québec, 2016-2017
2014-2015 | 2015-2016 | 2016-2017 | |
|---|---|---|---|
| Participating facilities (N) | 68 | 73 | 82 |
| Admissions (N) | 499,604 | 567,972 | 650,557 |
| Patient days (N) | 3,521,830 | 3,858,658 | 4,448,999 |
| Healthcare-associated BGNPC infections (cat. 1a and 1b) (N) | 9 | 5 | 17 |
| Healthcare-associated BGNPC colonizations (cat. 1a and 1b) (N) | 56 | 73 | 253 |
| Infected patients (cat. 1a and 1b) (N) | 8 | 5 | 15 |
Incidence rate
In 2016–2017, the incidence rate of HA-CPGNB infection (cat. 1a and 1b) is 0.04 per 10,000 patient days in all participating healthcare facilities (Table 2). Incidence rate of HA-CPGNB infection in non-teaching facilities is comparable to the one in teaching facilities (Table 2).
Table 2 – Incidence Rate and Percentile Distribution of Healthcare-Associated CPGNB Infection (Cat. 1a and 1b) by Type of Healthcare Facility, Québec, 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
| Healthcare facility vocation | Min. | 25% | 50% | 75% | 90% | Max. | Incidence rate |
|---|---|---|---|---|---|---|---|
| Non-teaching (N = 59) | 0 | 0 | 0 | 0.12 | 0.24 | 0.66 | 0.03 [0.01 ; 0.07] |
| Teaching (N = 23) | 0 | 0 | 0 | 0.14 | 0.2 | 0.43 | 0.04 [0.02 ; 0.08] |
| Total (N = 82) | 0 | 0 | 0 | 0.12 | 0.24 | 0.66 | 0.04 [0.03 ; 0.06] |
[95% CI]: 95% confidence interval.
Incidence rate trends
Among the 62 healthcare facilities participating in the three years of surveillance, the incidence rate of HA-CPGNB infections in 2016-2017 is 0.03 per 10,000 patient days and it doubled as compare to the one observed in 2015-2016 (Table 3). However, this difference is not statistically significant.
Table 3 – Change in Incidence Rate of Healthcare-Associated CPGNB infection (Cat. 1a and 1b) by Type of Healthcare Facility, Québec, 2014-2015 to 2016–2017 (Incidence Rate per 10,000 Patient Days [95% CI])
| Healthcare facility vocation | 2014-2015 | 2015-2016 | 2016-2017 | |||
|---|---|---|---|---|---|---|
Infections (N) | Incidence rate | Infections (N) | Incidence rate | Infections (N) | Incidence rate | |
| Non-teaching (N = 42) | 1 | 0.01 [0.00 ; 0.04] | 1 | 0.01 [0.00 ; 0.04] | 3 | 0.02 [0.01 ; 0.06] |
| Teaching (N = 20) | 8 | 0.04 [0.02 ; 0.08] | 4 | 0.02 [0.01 ; 0.05] | 6 | 0.03 [0.01 ; 0.07] |
| Total (N = 62) | 9 | 0.03 [0.02 ; 0.05] | 5 | 0.01 [0.00 ; 0.04] | 9 | 0.03 [0.02 ; 0.05] |
Note : Les données analysées sont celles des installations ayant participé à la surveillance de chaque année entre 2014-2015 et 2016-2017
Description of cases
A total of 29 infections (including 18 infections among new carriers) and 336 BGNPC colonizations are reported. Of the infections, 19 (65.5%) are healthcare associated, acquired either during a current hospitalization (16 infections, 9 in new carriers), a previous hospitalization (one in a new carrier) or ambulatory care (two in new carriers) of a reporting facility (cat. 1a, 1b and 1c). Ten infections (including six infections in new carriers) are related to a stay in a non-reporting facility, are community-associated or of unknown origin (cat. 2, 3 and 4).
Among the colonizations, 267 (79.5%) are acquired during a current hospitalization (207 colonizations and 9 infections in new carriers), a previous hospitalization (36 colonizations and one infection in a new carrier), or ambulatory care of reporting facilities (12 colonizations and two infections in new carriers) (cat. 1a, 1b and 1c). One colonization is observed among long-term care patients in the reporting facility (category 1d). Sixty eight (68) colonizations (including six infections in new carriers) are related to a stay in a non-reporting facility, are community-associated or of unknown origin (cat. 2, 3 and 4) (Table 4).
Table 4 – Cases of CPGNB Infections and Colonizations by Presumed Origin of Acquisition, Québec, 2016–2017 (N, %)
Category | Origin of acquisition | Infections | Colonizations | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
1a | Healthcare-associated with a current hospitalizationin the reporting facility | 16 | 55.2 | 216 | 65.1 |
1b | Healthcare-associated with a previous hospitalization in the reporting facility | 1 | 3.4 | 37 | 11.3 |
1c | Healthcare-associated with ambulatory care in the reporting facility | 2 | 6.9 | 14 | 3.8 |
1d | Healthcare-associated with long term unit in the reporting facility | 0 | 0.0 | 1 | 0.3 |
1e | Healthcare-associated with psychiatry unit in the reporting facility | 0 | 0.0 | 0 | 0.0 |
2 | Healthcare-associated with another facility | 4 | 13.8 | 21 | 5.7 |
3 | Community-associated | 5 | 17.2 | 34 | 10.1 |
4 | Unknown origin | 1 | 3.4 | 13 | 3.8 |
| Total | 29 | 100.0 | 336 | 100.0 |
Note: Colonizations included infections in new carriers.
In 2016-2017, three primary bloodstream infections (BSI) and three secondary bloodstream infections are reported among the 29 infections (Table 5).
Table 5 – Number of Cases of CPGNB Infections from All Origins by Type of Infection and Number of all Origin CPGNB Secondary BSIs , Québec, 2016–2017 (N = 29)
| Infection categories | Infection types | Infections (N) | Secondary bloodstream infections (N) |
|---|---|---|---|
| Primary BSI | CRBSI-MBI | 1 | - |
| CRBSI | 1 | - | |
| Non-CRBSI | 1 | - | |
| HD | 0 | - | |
| Primary infections | Urinary tract | 11 | 1 |
| Abdominal | 0 | 0 | |
| Pulmonary | 6 | 2 | |
| Surgical site | 1 | 0 | |
| Skin and soft tissues | 6 | 0 | |
| Bones and joints | 1 | 0 | |
| Others | 1 | 0 | |
| Total | 29 | 3 |
BSI: bloodstream infection
CRBSI: catheter-related bloodstream infection.
MBI: mucosal barrier injury.
Non-CRBSI: non-catheter-related primary bloodstream infection.
HD: hemodialysis.
A total of three deaths within 30 days are observed following onset of infection (Table 6).
Table 6 – Number of Deaths and 30-days all Cause Case-fatality in Patients Infected by a CPGNB, Québec, 2016-2017
2014-2015 | 2015-2016 | 2016-2017 | |
|---|---|---|---|
| CPGNB infections (all origins) | 13 | 8 | 29 |
| Number of deaths | 5 | 0 | 3 |
| Case fatality | 38.5 % | 0 % | 10.3 % |
In the vast majority of cases (221/347 = 63.7%), contact information is missing. When specified, the majority of colonizations occur following extended contact with a known carrier of the same gene within the last three weeks or during an outbreak, whereas this is the case for all infections. Nosocomial colonizations are more related to the presence of contact whereas non-nosocomial colonizations are more related to geographic risk factors.
Table 7 – Characteristics Associated With CPGNB Colonizations and Infections, Québec, 2016-2017
| Characteristics | Healthcare-associated colonizations | Healthcare-associated infections | Not healthcare-associated olonizations | Not healthcare0associated infections | ||
|---|---|---|---|---|---|---|
New carrier | Known carrier | New carrier | Known carrier | |||
| N | 243 | 10 | 7 | 75 | 8 | 4 |
| Type of contact | ||||||
| Contact not specified* | 138 | 6 | 2 | 65 | 6 | 4 |
| Close contact (24 hours in the same room) with a known carrier of the same gene during the last three weeks | 6 | 0 | 0 | 2 | 0 | 0 |
| Extended contact (24 hours in the same unit) with a known carrier of the same gene during the last three weeks | 85 | 4 | 2 | 6 | 2 | 0 |
| Outbreak occurring with the same gene in the healthcare facility | 14 | 0 | 3 | 2 | 0 | 0 |
| Geographic risk factors | ||||||
| Travel outside of Canada in the last 12 months | 1 | 0 | 0 | 17 | 3 | 1 |
| Health care aboard with or without hospitalization | 0 | 0 | 0 | 1 | 0 | 0 |
| Hospitalization outside Quebec over the last 12 months | 1 | 0 | 0 | 14 | 3 | 1 |
| Health care outside Quebec in the last 12 months | 0 | 0 | 0 | 2 | 1 | 1 |
| Patient residing in a long-term care hospital | 1 | 0 | 0 | 8 | 2 | 1 |
| Other characteristics | ||||||
| Active hematologic neoplasia | 7 | 1 | 0 | 0 | 0 | 0 |
| Neutropenia (<500 /mm³) | 6 | 2 | 0 | 0 | 0 | 0 |
| Hemofiltration | 2 | 0 | 0 | 1 | 1 | 0 |
| Autologous bone marrow transplant (< 3 months) | 0 | 0 | 0 | 0 | 0 | 0 |
| Allogenic bone marrow transplant | 0 | 0 | 0 | 0 | 0 | 0 |
| Solid organ transplant | 7 | 0 | 1 | 1 | 1 | 0 |
| Non hematological neoplasia | 25 | 2 | 0 | 1 | 0 | 0 |
| Diabetes | 44 | 3 | 1 | 23 | 2 | 0 |
| Acute renal failure | 14 | 0 | 1 | 4 | 0 | 0 |
| Chronic renal failure | 18 | 0 | 0 | 7 | 3 | 0 |
| Hyperalimentation IV (< 72h before infection) | 3 | 0 | 0 | 0 | 0 | 0 |
| No characteristic | 0 | 0 | 0 | 0 | 0 | 0 |
* None of the three contact types (close, extended or outbreak) has been specified.
Note: In order to detail the characteristics of the colonizations, the latter does not include infections in new carriers.
Note: The different contact types are mutually exclusive. In the situation where more than one contact is specified, the closest contact is selected.
Note: colonizations and nosocomial infections refer to categories 1a and 1b.
Note: Known carriers: infections from already known patients carrying the same gene.
Note: New carriers: infections from patients not known carrier or carrier of a new gene
.
Colonization Screening Protocol
In 2016-2017, the acquisition rate of HA-CPGNB colonization (cat. 1a and 1b) is 0.47 per 10,000 patient days among the 62 healthcare facilities participating in the three years surveillance (Table 8) and it is 0.53 per 10,000 patient days among all facilities in 2016-2017 (Table 13).
Table 8 – Change in the Number of Cases and Acquisition Rate of Healthcare-associated CPGNB Colonization (Cat. 1a and 1b) by Type of Healthcare Facility, Québec, 2014-2015 to 2015-2016 (Acquisition Rate of Healthcare-Associated CPGNB Colonization per 10,000 patient days)
| Healthcare facilities vocation | 2014-2015 | 2015-2016 | 2016-2017 | |||
|---|---|---|---|---|---|---|
Colonizations (N) | Acquisition rate | Colonizations (N) | Acquisition rate | Colonizations (N) | Acquisition rate | |
| Non-teaching (N = 42) | 33 | 0.22 | 50 | 0.34 | 59 | 0.37 |
| Teaching (N = 20) | 23 | 0.12 | 23 | 0.12 | 108 | 0.56 |
| Total (N = 62) * | 56 | 0.16 | 73 | 0.17 | 167 | 0.47 |
Note : Number of facilities participating in the three years surveillance.
* Significant difference (p < 0.05) between acquisition rate of 2015-2016 and 2016-2017.
Table 9 shows the number of non-teaching facilities that indicate the type of screening used at admission (non-teaching: 47 out of 59; teaching: 19 out of 23) and during hospitalization (non-teaching: 40 out of 59; teaching: 20 out of 23).
Table 9 – Number of Healthcare Facilities that Indicated the Type of Screening Procedure Used at Admission and During Hospitalization by Type of Facility, Québec, 2016-2017
Number of facilities that specified the type of screening procedure used* | ||||
|---|---|---|---|---|
At admission | During hospitalization | Not specified | Total | |
| Non-teaching (N = 59) | 47 | 40 | 15 | 51 |
| Teaching (N = 23) | 19 | 20 | 4 | 23 |
| Total (N = 82) | 66 | 60 | 19 | 74 |
* The "at admission" and "during hospitalization" categories are not mutually exclusives.
Tables 10 and 11 feature the total number of screening tests performed at admission and during hospitalization, as well as the mean number of CPGNB screening tests per admission. In 2015-2016, the total number of screening tests is 64,302, while the average number of screening tests is 0.124. In 2016-2017, this represents an increase of 196% for the total number of screening tests and 142% for the average of the screening tests.
Table 10 – Total Number of Screening Tests Performed at Admission and During Hospitalization by Type of Healthcare Facility, Québec, 2016-2017
| Healthcare facility vocations | Number of screening tests | |||
|---|---|---|---|---|
At admission | During hospitalization | Not specified | Total | |
| Non-teaching | 23,943 | 38,575 | 3,383 | 65,901 |
| Teaching | 29,650 | 86,847 | 11,674 | 128,171 |
| Total | 53,593 | 125,422 | 15,057 | 194,072 |
Table 11 – Mean Number of CPGNB Screening Tests by Type of Healthcare Facility, Québec, 2016-2017 (Mean CPGNB Screening Tests per Admission)
| Healthcare facility vocations | Mean number of CPGNB screening score* | ||
|---|---|---|---|
At admission | During hospitalization | Total | |
| Non-teaching | 0.07 | 0.11 | 0.2 |
| Teaching | 0.09 | 0.28 | 0.41 |
| Total | 0.08 | 0.19 | 0.30 |
* The "at admission" and "during hospitalization" categories are not mutually exclusives.
Microbiology
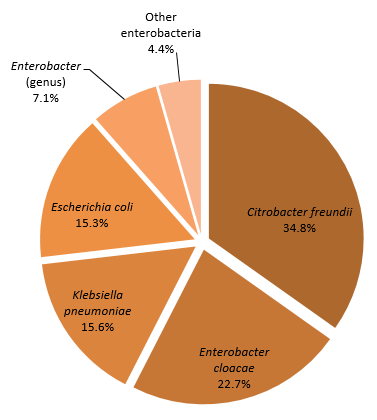
Figure 1 features the distribution of microorganisms isolated from all cases. A total of 360 microorganisms are isolated from 347 colonization and infection cases. The most frequently isolated microorganisms are Citrobacter freundii (34.8%), Enterobacter cloacae (22.7%), Klebsiella pneumoniae (15.6%) and Escherichia coli (15.3%). In two cases of colonization, three and four different microorganisms are isolated. In 22 cases, two microorganisms are isolated. Of these, four became infected.
Figure 1 – Categories of Isolated Microorganisms for all Cases (n = 347), Québec, 2016-2017
Isolated Microorganisms - All Cases (n = 359)
Table 12 shows the gene encoding carbapenemase identified in the various isolated microorganisms. The vast majority of the resistance genes linked to the various microorganisms is of the KPC type. Five strains of Escherichia coli, four strains of Klebsiella pneumoniae, one Citrobacter freudii strain and one strain of another enterobacterium carry the NDM gene. A strain of Klebsiella pneumoniae and a strain of Escherichia Coli carry both NDM and OXA-48 genes whereas a strain of Enterobacter cloacae bears both IMP and IMI / NMC genes.
Table 12 – Distribution of Carbapenemase-encoding Genes from Reported Microorganisms, Québec, 2016-2017
| Gene | Microorganism | |||
|---|---|---|---|---|
| Name | % | Name | N | % |
| KPC | 69.1 | Citrobacter freundii | 89 | 35.9 |
| Enterobacter cloacae | 45 | 18.1 | ||
| Klebsiella pneumoniae | 42 | 16.9 | ||
| Escherichia coli | 26 | 10.5 | ||
| Enterobacter (genus) | 23 | 9.3 | ||
| Klebsiella oxytoca | 9 | 3.6 | ||
| Serratia marcescens | 3 | 1.2 | ||
| Other enterobacteria | 11 | 4.4 | ||
| 248 | ||||
| OXA-48 | 15.3 | Citrobacter freundii | 27 | 49.1 |
| Escherichia coli | 20 | 36.4 | ||
| Klebsiella pneumoniae | 6 | 10.9 | ||
| Klebsiella oxytoca | 1 | 1.8 | ||
| Enterobacter (genus) | 1 | 1.8 | ||
| 55 | ||||
| IMI/NMC | 8.9 | Enterobacter cloacae | 30 | 93.8 |
| Enterobacter (genus) | 2 | 6.3 | ||
| 32 | ||||
| NDM | 3.1 | Escherichia coli | 5 | 45.5 |
| Klebsiella pneumoniae | 4 | 36.4 | ||
| Citrobacter freundii | 1 | 9.1 | ||
| Other enterobacteria | 1 | 9.1 | ||
| 11 | ||||
| SME | 1.9 | Serratia marcescens | 7 | 100 |
| 7 | ||||
| OXA48/NDM | 0.6 | Klebsiella pneumoniae | 1 | 50 |
| Escherichia coli | 1 | 50 | ||
| 2 | ||||
| VIM | 0.6 | Citrobacter freundii | 1 | 50 |
| Other enterobacteria | 1 | 50 | ||
| 2 | ||||
| IMP | 0.3 | Enterobacter cloacae | 1 | 100 |
| 1 | ||||
| IMP/IMI_NMC | 0.3 | Enterobacter cloacae | 1 | 100 |
| 1 | ||||
| Total | 359 |
KPC: Klebsiella pneumoniae carbapenemase (class A).
OXA-48: Family of Oxacillinase-48 (Class D) genes.
IMI/NMC: Imipenem-hydrolysing B-lactamase / Not metalloenzyme carbapenemase.
NDM: New-dehli metallo-β-lactamase (Class B).
SME: Serratia marcescens enzyme.
IMP: Imipenemase (IMP) metallo-β-lactamase
VIM : Verona imipenemase
Data per facility
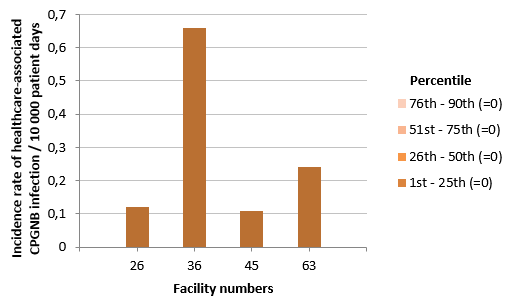
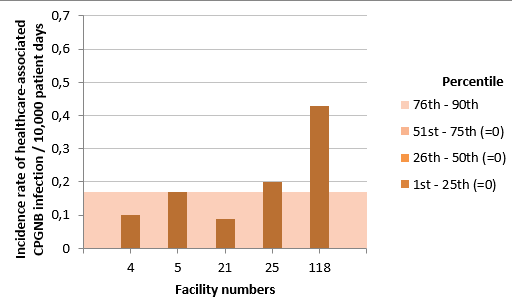
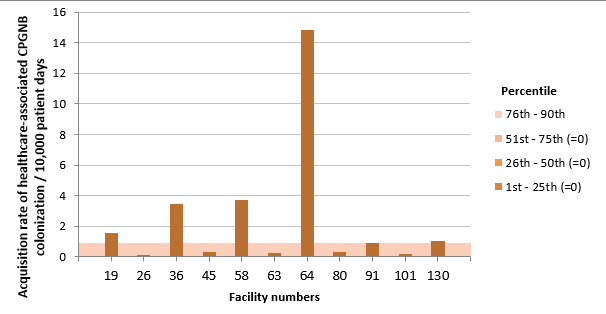
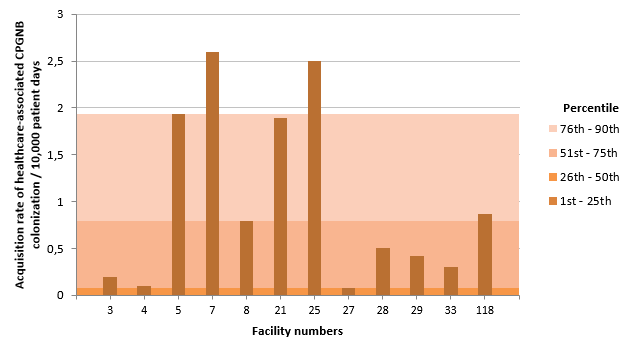
The incidence rate of HA-CPGNB infection and the percentile rankings by type of facility are shown in figures 2 and 3. Figures 4 and 5 present the rate of acquisition of HA-CPGNB colonization by type of facility.
Figure 2 – Incidence Rate and Percentile Ranking of Healthcare-Associated CPGNB infection (Cat. 1a and 1b) for Non-Teaching Healthcare Facilities, Québec, 2016-2017 (Incidence Rate per 10,000 Patient Days)
Note: Facilities 9, 10, 11, 14, 16, 19, 23, 32, 34, 35, 37, 38, 39, 40, 41, 42, 44, 46, 47, 49, 52, 53, 56, 58, 59, 61, 64, 65, 67, 70, 71, 72, 74, 75, 77, 80, 81, 82, 84, 85, 86, 88, 89, 91, 97, 99, 100, 101, 103, 107, 109, 111, 112, 113 and 130 did not report any cases of infection in 2016-2017.
Figure 3 – Incidence Rate and Percentile Ranking of Healthcare-Associated CPGNB Infection (Cat. 1a and 1b) for Teaching Healthcare Facilities, Québec, 2016-2017 (Incidence Rate per 10,000 Patient Days)
Note: Facilities 2, 3, 6, 7, 8, 13, 15, 18, 20, 22, 24, 27, 28, 29, 30, 31, 33 and 48 did not report any cases of infection in 2016-2017.
Figure 4 – Acquisition Rate of Healthcare-Associated CPGNB Colonization (Cat.1a and 1b) for Non-Teaching Healthcare Facilities, Québec, 2016-2017 (Acquisition Rate of Healthcare-Associated CPGNB Colonization per 10,000 Patient Days)
Note: Facilities 9, 10, 11, 14, 16, 23, 32, 34, 35, 37, 38, 39, 40, 41, 42, 44, 46, 47, 49, 52, 53, 56, 59, 61, 65, 67, 70, 71, 72, 74, 75, 77, 81, 82, 84, 85, 86, 88, 89, 97, 99, 100, 103, 107, 109, 111, 112 and 113 did not report any cases of colonization in 2016-2017.
Figure 5 – Acquisition Rate of Healthcare-Associated CPGNB Colonization (Cat.1a and 1b) for Teaching Healthcare Facilities, Québec, 2016-2017 (Acquisition Rate of Healthcare-Associated CPGNB Colonization per 10,000 Patient Days)
Note: Facilities 2, 6, 13, 15, 18, 20, 22, 24, 30, 31 and 48 did not report any cases of colonization in 2016-2017.
At the facility level, in 2016-2017, the incidence rate of HA-CPGNB infections ranges from 0 to 0.66 per 10,000 patient days, whereas the acquisition rate of HA-CPGNB colonization ranges from 0 to 14.83 per 10,000 patient days. A total of 59 facilities (71.9%) did not report any HA-CPGNB infection or colonization in 2016-2017. A detailed summary of the surveillance data for HA-CPGNB infection by healthcare facility can be found in table 13.
Table 13 – Incidence Rate of Healthcare-Associated CPGNB Infection (cat. 1a and 1b), Acquisition Rate of Healthcare-Associated CPGNB Colonization and Mean CPGNB Screening Tests by Admission and by Facility, Québec, 2016-2017 (Incidence Rate per 10,000 Patient Days [95% CI]; Acquisition Rate of Colonization per 10,000 Patient Days)
HR | Facility | Incidence rate of CPGNB infection (cat. 1a+1b) [95% CI] (N) | Acquisition rate of HA-CPGNB colonization (cat. 1a+1b) [95% CI] (N) | Mean CPGNB screening tests per admission* | |
|---|---|---|---|---|---|
Number | Name | ||||
1 | 16 | HÔPITAL RÉGIONAL DE RIMOUSKI | 0 | 0 | 0.13 |
32 | CENTRE HOSPITALIER RÉGIONAL DU GRAND-PORTAGE | 0 | 0 | 0.05 | |
61 | HÔPITAL NOTRE-DAME-DE-FATIMA | 0 | 0 | 0.05 | |
71 | HÔPITAL DE MATANE | 0 | 0 | 0.22 | |
77 | HÔPITAL D'AMQUI | 0 | 0 | 0 | |
84 | HÔPITAL DE NOTRE-DAME-DU-LAC | 0 | 0 | 0.08 | |
|
| BAS-SAINT-LAURENT | 0 | 0 | 0.11 |
2 | 20 | HÔPITAL DE CHICOUTIMI | 0 | 0 | 0.04 |
67 | HÔPITAL ET CENTRE DE RÉADAPTATION DE JONQUIÈRE | 0 | 0 | 0.01 | |
74 | HÔPITAL DE DOLBEAU-MISTASSINI | 0 | 0 | 0.01 | |
88 | HÔPITAL. CLSC ET CENTRE D'HÉBERGEMENT DE ROBERVAL | 0 | 0 | 0.01 | |
100 | HÔPITAL DE LA BAIE | 0 | 0 | 0.01 | |
112 | HÔPITAL D'ALMA | 0 | 0 | 0.01 | |
|
| SAGUENAY–LAC-SAINT-JEAN | 0 | 0 | 0.02 |
3 | 2 | HÔPITAL DE L'ENFANT-JÉSUS | 0 | 0 | 0.29 |
7 | PAVILLON L'HÔTEL-DIEU DE QUÉBEC | 0 | 2.60 [1.71 ; 3.95] (22) | 1.19 | |
24 | HÔPITAL DU SAINT-SACREMENT | 0 | 0 | 0.38 | |
27 | PAVILLON CENTRE HOSPITALIER DE L'UNIVERSITÉ LAVAL | 0 | 0.08 [0.01 ; 0.56] (1) | 0.22 | |
28 | PAVILLON SAINT-FRANCOIS D'ASSISE | 0 | 0.50 [0.21 ; 1.21] (5) | 0.38 | |
33 | INSTITUT UNIVERSITAIRE DE CARDIOLOGIE ET DE PNEUMOLOGIE DE QUÉBEC | 0 | 0.30 [0.10 ; 0.93] (3) | 0.36 | |
59 | HÔPITAL DE BAIE-SAINT-PAUL | 0 | 0 | 0.07 | |
86 | HÔPITAL DE LA MALBAIE | 0 | 0 | 0.05 | |
|
| CAPITALE-NATIONALE | 0 | 0.51 [0.36 ; 0.72] (31) | 0.4 |
4 | 23 | HÔTEL-DIEU D'ARTHABASKA | 0 | 0 | 0.01 |
31 | PAVILLON SAINTE-MARIE | 0 | 0 | 0 | |
41 | HÔPITAL DU CENTRE-DE-LA-MAURICIE | 0 | 0 | 0 | |
44 | HÔPITAL SAINTE-CROIX | 0 | 0 | 0.06 | |
85 | CENTRE DE SANTÉ ET DE SERVICES SOCIAUX DU HAUT-SAINT-MAURICE | 0 | 0 | 0.03 | |
|
| MAURICIE ET CENTRE-DU-QUÉBEC | 0 | 0 | 0.01 |
5 | 15 | HÔPITAL FLEURIMONT | 0 | 0 | 0 |
30 | HOTEL-DIEU DE SHERBROOKE | 0 | 0 | 0 | |
46 | HÔPITAL DE GRANBY | 0 | 0 | 0 | |
49 | CENTRE DE SANTÉ ET DE SERVICES SOCIAUX MEMPHRÉMAGOG | 0 | 0 | 0 | |
75 | CENTRE DE SANTÉ ET DE SERVICES SOCIAUX DU GRANIT | 0 | 0 | 0 | |
99 | HÔPITAL BROME-MISSISQUOI-PERKINS | 0 | 0 | 0 | |
| ESTRIE | 0 | 0 | 0 | |
6 | 3 | GLEN - ROYAL VICTORIA | 0 | 0.19 [0.05 ; 0.73] (2) | 0.17 |
4 | HÔPITAL NOTRE-DAME DU CHUM | 0.10 [0.02 ; 0.66] (1) | 0.10 [0.02 ; 0.66] (1) | 0.24 | |
5 | HÔPITAL GÉNÉRAL JUIF | 0.17 [0.05 ; 0.53] (3) | 1.94 [1.39 ; 2.71] (34) | 1.51 | |
6 | GLEN - ENFANTS | 0 | 0 | 0.09 | |
8 | PAVILLON MAISONNEUVE/PAVILLON MARCEL-LAMOUREUX | 0 | 0.79 [0.48 ; 1.31] (15) | 0.21 | |
12 | CENTRE HOSPITALIER UNIVERSITAIRE SAINTE-JUSTINE | - | - | - | |
13 | INSTITUT DE CARDIOLOGIE DE MONTRÉAL | 0 | 0 | 0.17 | |
21 | HÔPITAL SAINT-LUC DU CHUM | 0.09 [0.01 ; 0.71] (1) | 1.89 [1.22 ; 2.93] (20) | 0.45 | |
22 | HÔTEL-DIEU DU CHUM | 0 | 0 | 0.27 | |
25 | HÔPITAL DU SACRÉ-COEUR DE MONTRÉAL | 0.20 [0.07 ; 0.61] (3) | 2.5 [1.82 ; 3.43] (38) | 1.6 | |
26 | HÔPITAL DE VERDUN | 0.12 [0.02 ; 0.87] (1) | 0.12 [0.02 ; 0.87] (1) | 0.03 | |
29 | HÔPITAL GÉNÉRAL DE MONTRÉAL | 0 | 0.42 [0.14 ; 1.30] (3) | 0.34 | |
34 | HÔPITAL SANTA CABRINI | 0 | 0 | 0.02 | |
36 | HÔPITAL GÉNÉRAL DU LAKESHORE | 0.66 [0.27 ; 1.59] (5) | 3.45 [2.35 ; 5.07] (26) | 1.06 | |
38 | HÔPITAL JEAN-TALON | 0 | 0 | 0.61 | |
48 | CENTRE HOSPITALIER DE ST. MARY | 0 | 0 | 0.09 | |
76 | HOPITAL DE LACHINE | - | - | - | |
80 | HÔPITAL FLEURY | 0 | 0.34 [0.05 ; 2.37] (1) | 1.1 | |
83 | HÔPITAL DE LASALLE | - | - | - | |
118 | HÔPITAL NEUROLOGIQUE DE MONTRÉAL | 0.43 [0.06 ; 3.11] (1) | 0.87 [0.22 ; 3.47] (2) | 0.24 | |
| MONTRÉAL | 0.11 [0.07 ; 0.18] (15) | 1.00 [0.85 ; 1.18] (143) | 0.62 | |
7 | 39 | HÔPITAL DE GATINEAU | 0 | 0 | 0 |
40 | HÔPITAL DE HULL | 0 | 0 | 0.11 | |
51 | HÔPITAL DE MANIWAKI | - | - | - | |
95 | HÔPITAL DU PONTIAC | - | - | - | |
111 | HÔPITAL DE PAPINEAU | 0 | 0 | 0.02 | |
| OUTAOUAIS | 0 | 0 | 0.04 | |
8 | 47 | HÔPITAL DE ROUYN-NORANDA | 0 | 0 | 0.01 |
52 | HÔPITAL D'AMOS | 0 | 0 | 0 | |
65 | HÔPITAL ET CLSC DE VAL-D'OR | 0 | 0 | 0.02 | |
70 | CENTRE DE SOINS DE COURTE DURÉE LA SARRE | 0 | 0 | 0 | |
82 | PAVILLON SAINTE-FAMILLE | 0 | 0 | 0.13 | |
|
| ABITIBI-TÉMISCAMINGUE | 0 | 0 | 0.02 |
64 | HÔPITAL LE ROYER | 0 | 14.83 [9.46 ; 23.25] (19) | 1.64 | |
9 | 72 | HÔPITAL ET CENTRE D'HÉBERGEMENT DE SEPT-ÎLES | 0 | 0 | 0.03 |
|
| CÔTE-NORD | 0 | 9.76 [6.22 ; 15.30] (19) | 1.1 |
10 | 96 | CENTRE DE SANTÉ DE CHIBOUGAMAU | - | - | - |
|
| NORD-DU-QUÉBEC | - | - | - |
11 | 53 | HÔPITAL DE CHANDLER | 0 | 0 | 0 |
91 | HÔPITAL HÔTEL-DIEU DE GASPÉ | 0 | 0.90 [0.13 ; 6.36] (1) | 0.58 | |
97 | HÔPITAL DE MARIA | 0 | 0 | 0.08 | |
107 | HÔPITAL DE L'ARCHIPEL | 0 | 0 | 0.22 | |
109 | HÔPITAL DE SAINTE-ANNE-DES-MONTS | 0 | 0 | 0.13 | |
|
| GASPÉSIE–ÎLES-DE-LA-MADELEINE | 0 | 0.18 [0.03 ; 1.22] (1) | 0.19 |
12 | 18 | HÔTEL-DIEU DE LÉVIS | 0 | 0 | 0.16 |
63 | HÔPITAL DE SAINT-GEORGES | 0.24 [0.03 ; 1.73] (1) | 0.24 [0.03 ; 1.73] (1) | 0.79 | |
89 | HÔPITAL DE MONTMAGNY | 0 | 0 | 0.03 | |
113 | HÔPITAL DE THETFORD MINES | 0 | 0 | 0.03 | |
| CHAUDIÈRE-APPALACHES | 0.06 [0.01 ; 0.44] (1) | 0.06 [0.01 ; 0.44] (1) | 0.28 | |
13 | 19 | HÔPITAL CITÉ DE LA SANTÉ | 0 | 1.57 [1.09 ; 2.26] (29) | 0.37 |
|
| LAVAL | 0 | 1.57 [1.09 ; 2.26] (29) | 0.37 |
14 | 11 | HÔPITAL PIERRE-LE GARDEUR | 0 | 0 | 0.02 |
14 | CENTRE HOSPITALIER RÉGIONAL DE LANAUDIÈRE | 0 | 0 | 0 | |
|
| LANAUDIÈRE | 0 | 0 | 0.02 |
15 | 45 | HÔPITAL DE SAINT-EUSTACHE | 0.11 [0.02 ; 0.78] (1) | 0.33 [0.11 ; 1.02] (3) | 0.11 |
56 | CENTRE DE SANTÉ ET DE SERVICES SOCIAUX D'ARGENTEUIL | 0 | 0 | 0.32 | |
81 | HÔPITAL DE MONT-LAURIER | 0 | 0 | 0.16 | |
101 | HÔPITAL RÉGIONAL DE SAINT-JÉRÔME | 0 | 0.18 [0.04 ; 0.73] (2) | 0.12 | |
103 | HÔPITAL LAURENTIEN | 0 | 0 | 0.05 | |
|
| LAURENTIDES | 0.04 [0.01 ; 0.25] (1) | 0.19 [0.08 ; 0.45] (5) | 0.12 |
16 | 1 | HÔPITAL CHARLES LEMOYNE | - | - | - |
9 | HÔPITAL DU HAUT-RICHELIEU | 0 | 0 | 0.01 | |
10 | HÔPITAL PIERRE-BOUCHER | 0 | 0 | 0 | |
35 | HÔPITAL HONORÉ-MERCIER | 0 | 0 | 0.04 | |
37 | HÔTEL-DIEU DE SOREL | 0 | 0 | 0 | |
42 | CENTRE HOSPITALIER ANNA-LABERGE | 0 | 0 | 0.08 | |
58 | HÔPITAL DU SUROÎT | 0 | 3.69 [2.45 ; 5.55] (23) | 1.92 | |
130 | HÔPITAL BARRIE MEMORIAL | 0 | 1.04 [0.15 ; 7.32] (1) | 1.44 | |
| MONTÉRÉGIE | 0 | 0.51 [0.34 ; 0.76] (24) | 0.24 | |
| Total | 0.04 [0.03 ; 0.06] (17) | 0.57 [0.50 ; 0.64] (253) | 0.3 |
* Number of screening tests divided by number of admissions.
- Healthcare facilities that did not participate in 2016-2017.
HR : Health region.
Author
Comité de surveillance provinciale des infections nosocomiales (SPIN)
Editorial Committee
Christophe Garenc, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Christian Lavallée, Hôpital Maisonneuve-Rosemont
Danielle Moisan, Centre hospitalier régional du Grand-Portage
Muleka Ngenda-Muadi, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Isabelle Rocher, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Claude Tremblay, Centre hospitalier universitaire de Québec – Université Laval
Mélissa Trudeau, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Jasmin Villeneuve, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec